Monday Poster Session
Category: Liver
P2413 - Characteristics of Autoimmune Hepatitis in a Multicenter Network of Inflammatory Bowel Disease Patients
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- FJ
Fangyuan Jin-Dominguez, MD
Case Western Reserve / University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Fangyuan Jin-Dominguez, MD1, Khadija Naseem, MD2, Abbinaya Elangovan, MD3, Ahmad Khan, MD3, Jeffry Katz, MD3, Gregory Cooper, MD3, Yngve Falck-Ytter, MD4, Vu Nguyen, MD3
1Case Western Reserve / University Hospitals Cleveland Medical Center, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Case Western Reserve/UHCMC, Cleveland, OH; 4Case Western Reserve/Louis Stokes Cleveland VAMC, Cleveland, OH
Introduction: Autoimmune hepatitis (AIH) is a rare liver-related extraintestinal manifestation of inflammatory bowel disease (IBD). However, little is known about its prevalence and characteristics in patients with IBD. We aimed to study the prevalence, patient characteristics, and liver clinical course of AIH in IBD patients in a large multi-center patient database.
Methods: We conducted a retrospective cohort study using TriNetX (Cambridge, MA, USA), a multi-center health research network containing electronic health records across 54 US healthcare organizations. We identified a cohort of IBD patients with a concurrent diagnosis of AIH per ICD-10 codes from 1/1/2016 to 12/31/2021. Data on the prevalence of AIH, rate of concurrent primary sclerosing cholangitis (PSC), demographics, comorbidities, and liver outcomes were collected. We performed chi-square test for categorical and student T-test for continuous data. Propensity score matching was performed for demographics and comorbidities to evaluate for liver outcomes.
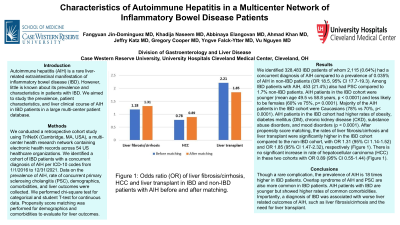
Results: We identified 328,483 IBD patients of whom 2,115 (0.64%) had a concurrent diagnosis of AIH compared to a prevalence of 0.035% of AIH in non-IBD patients (OR 18.5, 95% CI 17.7-19.3). Among IBD patients with AIH, 453 (21.4%) also had PSC compared to 1.7% non-IBD patients. AIH patients in the IBD cohort were younger (mean age 49.5 vs 58.8 years, p < 0.0001) and less likely to be females (60% vs 75%, p< 0.0001). Majority of the AIH patients in the IBD cohort were Caucasians (78% vs 70%, p< 0.0001) (Table 1). AIH patients in the IBD cohort had higher rates of obesity, diabetes mellitus (DM), chronic kidney disease (CKD), substance abuse disorders, and mood disorders (p < 0.0001) (Table 1). After propensity score matching, the rates of liver fibrosis/cirrhosis and liver transplant were significantly higher in the IBD cohort compared to the non-IBD cohort, with OR 1.31 (95% CI 1.14-1.52) and OR 1.85 (95% CI 1.47-2.32), respectively (Figure 1). There is no significant increase in rate of hepatocellular carcinoma (HCC) in these two cohorts with OR 0.89 (95% CI 0.55-1.44) (Figure 1).
Discussion: Though a rare complication, the prevalence of AIH is 18 times higher in IBD patients. Overlap syndrome of AIH and PSC are also more common in IBD patients. AIH patients with IBD are younger but showed higher rates of common comorbidities. Importantly, a diagnosis of IBD was associated with worse liver related outcomes of AIH, such as liver fibrosis/cirrhosis and the need for liver transplant.

Disclosures:
Fangyuan Jin-Dominguez, MD1, Khadija Naseem, MD2, Abbinaya Elangovan, MD3, Ahmad Khan, MD3, Jeffry Katz, MD3, Gregory Cooper, MD3, Yngve Falck-Ytter, MD4, Vu Nguyen, MD3. P2413 - Characteristics of Autoimmune Hepatitis in a Multicenter Network of Inflammatory Bowel Disease Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Case Western Reserve / University Hospitals Cleveland Medical Center, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Case Western Reserve/UHCMC, Cleveland, OH; 4Case Western Reserve/Louis Stokes Cleveland VAMC, Cleveland, OH
Introduction: Autoimmune hepatitis (AIH) is a rare liver-related extraintestinal manifestation of inflammatory bowel disease (IBD). However, little is known about its prevalence and characteristics in patients with IBD. We aimed to study the prevalence, patient characteristics, and liver clinical course of AIH in IBD patients in a large multi-center patient database.
Methods: We conducted a retrospective cohort study using TriNetX (Cambridge, MA, USA), a multi-center health research network containing electronic health records across 54 US healthcare organizations. We identified a cohort of IBD patients with a concurrent diagnosis of AIH per ICD-10 codes from 1/1/2016 to 12/31/2021. Data on the prevalence of AIH, rate of concurrent primary sclerosing cholangitis (PSC), demographics, comorbidities, and liver outcomes were collected. We performed chi-square test for categorical and student T-test for continuous data. Propensity score matching was performed for demographics and comorbidities to evaluate for liver outcomes.
Results: We identified 328,483 IBD patients of whom 2,115 (0.64%) had a concurrent diagnosis of AIH compared to a prevalence of 0.035% of AIH in non-IBD patients (OR 18.5, 95% CI 17.7-19.3). Among IBD patients with AIH, 453 (21.4%) also had PSC compared to 1.7% non-IBD patients. AIH patients in the IBD cohort were younger (mean age 49.5 vs 58.8 years, p < 0.0001) and less likely to be females (60% vs 75%, p< 0.0001). Majority of the AIH patients in the IBD cohort were Caucasians (78% vs 70%, p< 0.0001) (Table 1). AIH patients in the IBD cohort had higher rates of obesity, diabetes mellitus (DM), chronic kidney disease (CKD), substance abuse disorders, and mood disorders (p < 0.0001) (Table 1). After propensity score matching, the rates of liver fibrosis/cirrhosis and liver transplant were significantly higher in the IBD cohort compared to the non-IBD cohort, with OR 1.31 (95% CI 1.14-1.52) and OR 1.85 (95% CI 1.47-2.32), respectively (Figure 1). There is no significant increase in rate of hepatocellular carcinoma (HCC) in these two cohorts with OR 0.89 (95% CI 0.55-1.44) (Figure 1).
Discussion: Though a rare complication, the prevalence of AIH is 18 times higher in IBD patients. Overlap syndrome of AIH and PSC are also more common in IBD patients. AIH patients with IBD are younger but showed higher rates of common comorbidities. Importantly, a diagnosis of IBD was associated with worse liver related outcomes of AIH, such as liver fibrosis/cirrhosis and the need for liver transplant.

Figure: Figure 1: Odds ratio (OR) of liver fibrosis/cirrhosis, HCC and liver transplant in IBD and non-IBD patients with AIH before and after matching.
Disclosures:
Fangyuan Jin-Dominguez indicated no relevant financial relationships.
Khadija Naseem indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Ahmad Khan indicated no relevant financial relationships.
Jeffry Katz: Janssen, Pharmaceuticals – Grant/Research Support.
Gregory Cooper indicated no relevant financial relationships.
Yngve Falck-Ytter indicated no relevant financial relationships.
Vu Nguyen: AbbVie – Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member.
Fangyuan Jin-Dominguez, MD1, Khadija Naseem, MD2, Abbinaya Elangovan, MD3, Ahmad Khan, MD3, Jeffry Katz, MD3, Gregory Cooper, MD3, Yngve Falck-Ytter, MD4, Vu Nguyen, MD3. P2413 - Characteristics of Autoimmune Hepatitis in a Multicenter Network of Inflammatory Bowel Disease Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
