Monday Poster Session
Category: Liver
P2417 - Outcomes and Predictors of Liver Cirrhosis in Hereditary Hemochromatosis: A Population-based Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- CN
Chengu Niu, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Chengu Niu, MD1, Jing Zhang, MD2, Tausif Syed, MD1, Sheza Malik, MD1, Ali Jaan, MD1, Umer Farooq, MD1, Ahmed Shehadah, MD1, Harkarandeep Singh, MD1, Jay Bapaye, MD1, Karin Dunnigan, MD1
1Rochester General Hospital, Rochester, NY; 2Rainier Springs Hospital, Vancouver, WA
Introduction: Hereditary Hemochromatosis (HH), characterized by an elevated serum iron level, is linked with a significant risk of liver cirrhosis. This disease progression is associated with decreased quality of life and survival rate, creating an urgent need for research in this field. However, national-level studies investigating the risk factors and inpatient outcomes for liver cirrhosis in HH patients are scarce. Our study aims to fill this gap by examining the prevalence, predictors, and hospital-associated outcomes of liver cirrhosis in this population.
Methods: We used the National Inpatient Sample (NIS) database from October 2015 through December 2019 to identify patients diagnosed with HH and liver cirrhosis using ICD-10 codes. The cohort was divided into groups with and without liver cirrhosis. Adjusted odds ratios (AOR) for risk factors and outcomes were calculated using multivariate regression analysis, complemented by a weighted analysis using Stata 17.
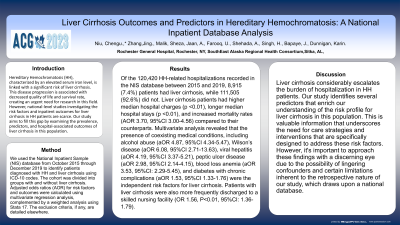
Results: Of the 120,420 HH-related hospitalizations recorded in the NIS database between 2015 and 2019, 8,915 (7.4%) patients had liver cirrhosis, while 111,505 (92.6%) did not. Liver cirrhosis patients had higher median hospital charges (p < 0.01), longer median hospital stays (p < 0.01), and increased mortality rates (AOR 3.70, 95%CI 3.00-4.56) compared to their counterparts. Multivariate analysis revealed that the presence of coexisting medical conditions, including alcohol abuse (aOR 4.87, 95%CI 4.34-5.47), Wilson’s disease (aOR 6.08, 95%CI 2.71-13.63), viral hepatitis (aOR 4.19, 95%CI 3.37-5.21), peptic ulcer disease (aOR 2.98, 95%CI 2.14-4.15), blood loss anemia (aOR 3.53, 95%CI: 2.29-5.45), and diabetes with chronic complications (aOR 1.53, 95%CI 1.33-1.76) were the independent risk factors for liver cirrhosis. Patients with liver cirrhosis were also more frequently discharged to a skilled nursing facility (OR 1.56, P< 0.01, 95%CI: 1.36-1.79).
Discussion: Liver cirrhosis considerably escalates the burden of hospitalization in HH patients. Our study identifies several predictors that enrich our understanding of the risk profile for liver cirrhosis in this population. This is valuable information that underscores the need for care strategies and interventions that are specifically designed to address these risk factors.

Disclosures:
Chengu Niu, MD1, Jing Zhang, MD2, Tausif Syed, MD1, Sheza Malik, MD1, Ali Jaan, MD1, Umer Farooq, MD1, Ahmed Shehadah, MD1, Harkarandeep Singh, MD1, Jay Bapaye, MD1, Karin Dunnigan, MD1. P2417 - Outcomes and Predictors of Liver Cirrhosis in Hereditary Hemochromatosis: A Population-based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Rainier Springs Hospital, Vancouver, WA
Introduction: Hereditary Hemochromatosis (HH), characterized by an elevated serum iron level, is linked with a significant risk of liver cirrhosis. This disease progression is associated with decreased quality of life and survival rate, creating an urgent need for research in this field. However, national-level studies investigating the risk factors and inpatient outcomes for liver cirrhosis in HH patients are scarce. Our study aims to fill this gap by examining the prevalence, predictors, and hospital-associated outcomes of liver cirrhosis in this population.
Methods: We used the National Inpatient Sample (NIS) database from October 2015 through December 2019 to identify patients diagnosed with HH and liver cirrhosis using ICD-10 codes. The cohort was divided into groups with and without liver cirrhosis. Adjusted odds ratios (AOR) for risk factors and outcomes were calculated using multivariate regression analysis, complemented by a weighted analysis using Stata 17.
Results: Of the 120,420 HH-related hospitalizations recorded in the NIS database between 2015 and 2019, 8,915 (7.4%) patients had liver cirrhosis, while 111,505 (92.6%) did not. Liver cirrhosis patients had higher median hospital charges (p < 0.01), longer median hospital stays (p < 0.01), and increased mortality rates (AOR 3.70, 95%CI 3.00-4.56) compared to their counterparts. Multivariate analysis revealed that the presence of coexisting medical conditions, including alcohol abuse (aOR 4.87, 95%CI 4.34-5.47), Wilson’s disease (aOR 6.08, 95%CI 2.71-13.63), viral hepatitis (aOR 4.19, 95%CI 3.37-5.21), peptic ulcer disease (aOR 2.98, 95%CI 2.14-4.15), blood loss anemia (aOR 3.53, 95%CI: 2.29-5.45), and diabetes with chronic complications (aOR 1.53, 95%CI 1.33-1.76) were the independent risk factors for liver cirrhosis. Patients with liver cirrhosis were also more frequently discharged to a skilled nursing facility (OR 1.56, P< 0.01, 95%CI: 1.36-1.79).
Discussion: Liver cirrhosis considerably escalates the burden of hospitalization in HH patients. Our study identifies several predictors that enrich our understanding of the risk profile for liver cirrhosis in this population. This is valuable information that underscores the need for care strategies and interventions that are specifically designed to address these risk factors.

Figure: Hemochromatosis without liver cirrhosis versus with liver cirrhosis
Disclosures:
Chengu Niu indicated no relevant financial relationships.
Jing Zhang indicated no relevant financial relationships.
Tausif Syed indicated no relevant financial relationships.
Sheza Malik indicated no relevant financial relationships.
Ali Jaan indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Harkarandeep Singh indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Karin Dunnigan indicated no relevant financial relationships.
Chengu Niu, MD1, Jing Zhang, MD2, Tausif Syed, MD1, Sheza Malik, MD1, Ali Jaan, MD1, Umer Farooq, MD1, Ahmed Shehadah, MD1, Harkarandeep Singh, MD1, Jay Bapaye, MD1, Karin Dunnigan, MD1. P2417 - Outcomes and Predictors of Liver Cirrhosis in Hereditary Hemochromatosis: A Population-based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
