Monday Poster Session
Category: Liver
P2422 - Mortality and Outcomes in Patients With NAFLD/NASH Following Clostridium difficile Infection
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ankoor Patel, MD
Rutgers-Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Ankoor Patel, MD1, Gaurav Pathak, PharmD1, Alexander Chen, MD2, Carlos Minacapelli, MD1, Carolyn Catalano, APN1, Vinod Rustgi, MD, MBA1
1Rutgers-Robert Wood Johnson Medical School, New Brunswick, NJ; 2Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Clostridium difficile (C. Diff) infection (CDI) is the most common cause of healthcare-associated diarrhea as its’ prevalence and mortality rate continues to rise. With the rising prevalence of obesity and metabolic disease, nonalcoholic fatty liver disease is increasingly more common and affects up to 25% of the adult population. Data on outcomes and mortality of CDI in NAFLD/NASH patients is scarce. Our study used the National Inpatient Sample (NIS) to evaluate hospital utilization, outcomes, and risk factors for mortality among patients with CDI and NAFLD/NASH.
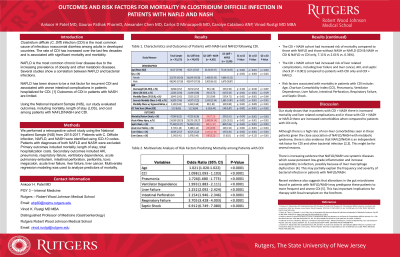
Methods: We performed a retrospective cohort study using the National Inpatient Sample (NIS) from 2015-2017. Patients with C. Difficile infection, NAFLD, and NASH were identified using ICD-10 codes. Patients with diagnoses of both NAFLD and NASH were excluded. Primary outcomes included mortality, length of stay, total hospitalization costs. Secondary outcomes included AKI, pneumonia, respiratory failure, ventilatory dependence, acute pulmonary embolism, intestinal perforation, peritonitis, toxic megacolon, acute liver failure, liver failure, liver cancer. Multivariate logistic regression analysis was used to compare the two groups.
Results: A total of 761,175 patients with CDI were included and 11,335 (1.49%) had NAFLD and 4,365 (0.57%) had NASH. Patients with CDI and NASH were at increased risk for liver related complications, including liver failure and liver cancer, acute kidney injury, and septic shock (P < 0.001) compared to patients with CDI only. Patients hospitalized for CDI with NASH had an increased risk of mortality compared to those with NAFLD and those without NASH or NAFLD (CDI & NASH vs CDI & NAFLD vs CDI only, 7.11% vs 2.61% vs. 6.36%). Multivariable regression analysis on mortality during hospitalization was performed and demonstrated higher odds of mortality in the following group: Age (OR 1.021; P < 0.0001), CCI (OR 1.098; P < 0.0001), Pneumonia (OR 1.726; P < 0.0001), Ventilator Dependence (OR 1.993; P < 0.0001), Liver failure (OR 2.252; P < 0.0001), Intestinal Perforation (OR 2.145; P < 0.0001), Respiratory Failure (OR 3.705; P < 0.0001), and Septic Shock (OR 6.912; P < 0.0001).
Discussion: Patients with NASH have a higher rate of mortality following CDI. AKI, septic shock, and liver-related complications following CDI. Septic shock, respiratory failure, intestinal perforation, liver failure, pneumonia, ventilatory dependence, CCI, and age increased the risk of death among patients with CDI.
Disclosures:
Ankoor Patel, MD1, Gaurav Pathak, PharmD1, Alexander Chen, MD2, Carlos Minacapelli, MD1, Carolyn Catalano, APN1, Vinod Rustgi, MD, MBA1. P2422 - Mortality and Outcomes in Patients With NAFLD/NASH Following Clostridium difficile Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rutgers-Robert Wood Johnson Medical School, New Brunswick, NJ; 2Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Clostridium difficile (C. Diff) infection (CDI) is the most common cause of healthcare-associated diarrhea as its’ prevalence and mortality rate continues to rise. With the rising prevalence of obesity and metabolic disease, nonalcoholic fatty liver disease is increasingly more common and affects up to 25% of the adult population. Data on outcomes and mortality of CDI in NAFLD/NASH patients is scarce. Our study used the National Inpatient Sample (NIS) to evaluate hospital utilization, outcomes, and risk factors for mortality among patients with CDI and NAFLD/NASH.
Methods: We performed a retrospective cohort study using the National Inpatient Sample (NIS) from 2015-2017. Patients with C. Difficile infection, NAFLD, and NASH were identified using ICD-10 codes. Patients with diagnoses of both NAFLD and NASH were excluded. Primary outcomes included mortality, length of stay, total hospitalization costs. Secondary outcomes included AKI, pneumonia, respiratory failure, ventilatory dependence, acute pulmonary embolism, intestinal perforation, peritonitis, toxic megacolon, acute liver failure, liver failure, liver cancer. Multivariate logistic regression analysis was used to compare the two groups.
Results: A total of 761,175 patients with CDI were included and 11,335 (1.49%) had NAFLD and 4,365 (0.57%) had NASH. Patients with CDI and NASH were at increased risk for liver related complications, including liver failure and liver cancer, acute kidney injury, and septic shock (P < 0.001) compared to patients with CDI only. Patients hospitalized for CDI with NASH had an increased risk of mortality compared to those with NAFLD and those without NASH or NAFLD (CDI & NASH vs CDI & NAFLD vs CDI only, 7.11% vs 2.61% vs. 6.36%). Multivariable regression analysis on mortality during hospitalization was performed and demonstrated higher odds of mortality in the following group: Age (OR 1.021; P < 0.0001), CCI (OR 1.098; P < 0.0001), Pneumonia (OR 1.726; P < 0.0001), Ventilator Dependence (OR 1.993; P < 0.0001), Liver failure (OR 2.252; P < 0.0001), Intestinal Perforation (OR 2.145; P < 0.0001), Respiratory Failure (OR 3.705; P < 0.0001), and Septic Shock (OR 6.912; P < 0.0001).
Discussion: Patients with NASH have a higher rate of mortality following CDI. AKI, septic shock, and liver-related complications following CDI. Septic shock, respiratory failure, intestinal perforation, liver failure, pneumonia, ventilatory dependence, CCI, and age increased the risk of death among patients with CDI.
Disclosures:
Ankoor Patel indicated no relevant financial relationships.
Gaurav Pathak indicated no relevant financial relationships.
Alexander Chen indicated no relevant financial relationships.
Carlos Minacapelli indicated no relevant financial relationships.
Carolyn Catalano indicated no relevant financial relationships.
Vinod Rustgi indicated no relevant financial relationships.
Ankoor Patel, MD1, Gaurav Pathak, PharmD1, Alexander Chen, MD2, Carlos Minacapelli, MD1, Carolyn Catalano, APN1, Vinod Rustgi, MD, MBA1. P2422 - Mortality and Outcomes in Patients With NAFLD/NASH Following Clostridium difficile Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
