Monday Poster Session
Category: Liver
P2452 - An Unusual Presentation of Progressive Thrombocytopenia and Splenomegaly Following Liver Transplantation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Agnieszka Maniak, MD
Rush University Medical Center
Chicago, Illinois
Presenting Author(s)
Agnieszka Maniak, MD, Nancy Reau, MD
Rush University Medical Center, Chicago, IL
Introduction: Nodular regenerative hyperplasia (NRH) is characterized by non-cirrhotic portal hypertension thought to be secondary to changes in hepatic blood flow. We present a rare case of progressive thrombocytopenia and splenomegaly post liver transplant concerning for NRH.
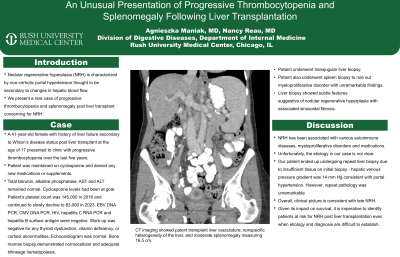
Case Description/Methods: A 41-year-old female with history of liver failure secondary to Wilson’s disease status post liver transplant at the age of 17 presented to clinic with progressive thrombocytopenia over the last five years and recent onset of fatigue. Patient was maintained on chronic immunosuppressive therapy with cyclosporine. Patient denied any new medications or supplements. Total bilirubin, alkaline phosphatase, AST and ALT remained normal. Cyclosporine levels had been at goal. Patient’s platelet count was 145,000 in 2018 and continued to slowly decline to 83,000 in 2023. EBV DNA PCR, CMV DNA PCR, HIV, hepatitis C RNA PCR and hepatitis B surface antigen were negative. Work-up was negative for any thyroid dysfunction, vitamin deficiency, or cortisol abnormalities. CT imaging showed patent transplant liver vasculature, nonspecific heterogeneity of the liver, and moderate splenomegaly measuring 16.5 centimeters. Echocardiogram showed normal systolic and diastolic function. Patient underwent bone marrow biopsy that demonstrated normocellular and adequate trilineage hematopoiesis. Given overall negative work-up, patient underwent transjugular liver biopsy. Although a small sample was obtained, liver biopsy showed subtle features suggestive of nodular regenerative hyperplasia with associated sinusoidal fibrosis. There was stage 2 periportal fibrosis. Patient also underwent spleen biopsy to rule out myeloproliferative disorder with unremarkable findings.
Discussion: NRH has been associated with various autoimmune diseases, myeloproliferative disorders and medications. Unfortunately, the etiology in our case is not clear. Devarbhavi et al. published a retrospective study where they identified (n = 7) patients with symptomatic NRH all of whom had vascular abnormalities on doppler ultrasonography - not present in our patient. Our patient ended up undergoing repeat liver biopsy due to insufficient tissue on initial biopsy - hepatic venous pressure gradient was 12 mm Hg consistent with portal hypertension. However, repeat pathology was unremarkable. Given its impact on survival, it is imperative to identify patients at risk for NRH post liver transplantation even when etiology and diagnosis are difficult to establish.

Disclosures:
Agnieszka Maniak, MD, Nancy Reau, MD. P2452 - An Unusual Presentation of Progressive Thrombocytopenia and Splenomegaly Following Liver Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Nodular regenerative hyperplasia (NRH) is characterized by non-cirrhotic portal hypertension thought to be secondary to changes in hepatic blood flow. We present a rare case of progressive thrombocytopenia and splenomegaly post liver transplant concerning for NRH.
Case Description/Methods: A 41-year-old female with history of liver failure secondary to Wilson’s disease status post liver transplant at the age of 17 presented to clinic with progressive thrombocytopenia over the last five years and recent onset of fatigue. Patient was maintained on chronic immunosuppressive therapy with cyclosporine. Patient denied any new medications or supplements. Total bilirubin, alkaline phosphatase, AST and ALT remained normal. Cyclosporine levels had been at goal. Patient’s platelet count was 145,000 in 2018 and continued to slowly decline to 83,000 in 2023. EBV DNA PCR, CMV DNA PCR, HIV, hepatitis C RNA PCR and hepatitis B surface antigen were negative. Work-up was negative for any thyroid dysfunction, vitamin deficiency, or cortisol abnormalities. CT imaging showed patent transplant liver vasculature, nonspecific heterogeneity of the liver, and moderate splenomegaly measuring 16.5 centimeters. Echocardiogram showed normal systolic and diastolic function. Patient underwent bone marrow biopsy that demonstrated normocellular and adequate trilineage hematopoiesis. Given overall negative work-up, patient underwent transjugular liver biopsy. Although a small sample was obtained, liver biopsy showed subtle features suggestive of nodular regenerative hyperplasia with associated sinusoidal fibrosis. There was stage 2 periportal fibrosis. Patient also underwent spleen biopsy to rule out myeloproliferative disorder with unremarkable findings.
Discussion: NRH has been associated with various autoimmune diseases, myeloproliferative disorders and medications. Unfortunately, the etiology in our case is not clear. Devarbhavi et al. published a retrospective study where they identified (n = 7) patients with symptomatic NRH all of whom had vascular abnormalities on doppler ultrasonography - not present in our patient. Our patient ended up undergoing repeat liver biopsy due to insufficient tissue on initial biopsy - hepatic venous pressure gradient was 12 mm Hg consistent with portal hypertension. However, repeat pathology was unremarkable. Given its impact on survival, it is imperative to identify patients at risk for NRH post liver transplantation even when etiology and diagnosis are difficult to establish.

Figure: CT abdomen and pelvis with IV contrast showing no focal liver mass, bile duct dilatation or ascites. CT does show splenomegaly without a focal mass.
Disclosures:
Agnieszka Maniak indicated no relevant financial relationships.
Nancy Reau: Abbott – Advisory Committee/Board Member. AbbVie – Advisory Committee/Board Member. Arbutus – Advisor or Review Panel Member. Gilead – Advisory Committee/Board Member. Salix – Advisory Committee/Board Member.
Agnieszka Maniak, MD, Nancy Reau, MD. P2452 - An Unusual Presentation of Progressive Thrombocytopenia and Splenomegaly Following Liver Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
