Monday Poster Session
Category: Liver
P2474 - Cardiac Ascites With an Unusual Presentation on Peritoneal Fluid Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Nikhil Furtado, BS
Creighton University School of Medicine
Omaha, NE
Presenting Author(s)
Nikhil Furtado, BS1, Suhail Sidhu, BS1, Thomas Checketts, DO1, Syed Mohsin Saghir, MD2, Rajani Rangray, MBBS1
1Creighton University School of Medicine, Omaha, NE; 2Creighton University, Omaha, NE
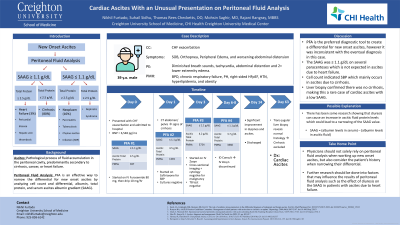
Introduction: Ascites is a pathological process of fluid accumulation in the peritoneal cavity predominantly secondary to cirrhosis, cancer, or heart failure. Peritoneal fluid analysis is an effective way to narrow the differential for new onset ascites by analyzing cell count and differential, albumin, total protein, and serum ascites albumin gradient (SAAG). Here we present a case where the typical diagnostic criteria for peritoneal fluid was inconsistent with the correct etiology.
Case Description/Methods: A 37-year-old man with past medical history of bronchopulmonary dysplasia, chronic respiratory failure on supplemental oxygen, pulmonary hypertension, right-sided HFpEF, hypertension, hyperlipidemia, and obesity presented with a congestive heart failure exacerbation. He reported worsening dyspnea, orthopnea, and peripheral edema for weeks. Physical exam revealed diminished breath sounds, tachycardia, abdominal distension, and 2 + lower extremity edema. Vitals included: T: 36.5 °C (97.7 °F), BP: 142/84, HR: 93, and SpO2: 95%. Given the abdominal distension, ascites was a concern. Paracentesis revealed 947 polymorphonuclear neutrophils (PMNs), which is diagnostic for spontaneous bacterial peritonitis, commonly occurring in cirrhosis. Cultures were negative. He was started on ceftriaxone then escalated to Zosyn due to increasing PMNs. SAAG was < 1.1 g/dl, suggesting ascites wasn’t due to portal hypertension, making heart failure and cirrhosis less likely. Ascites total protein and B-type natriuretic peptide were elevated at 4.5 g/dl and 6,548 pg/ml, respectively, consistent with heart failure. However, abdominal CT suggested cirrhosis, further confusing the picture. Cross-sectional imaging was negative for malignancy. He was discharged after his dyspnea, edema, and PMNs improved with intravenous furosemide and Zosyn. During outpatient follow-up with gastroenterology, a transjugular liver biopsy revealed normal histology with hepatic vein pressure gradient of 1 mmHg, excluding cirrhosis. Therefore, despite SAAG < 1.1 g/dl, it was deemed the ascites was secondary to the patient’s right-sided heart failure.
Discussion: While peritoneal fluid analysis is the preferred method to work-up new onset ascites, it is not always accurate. In this case, our patient's fluid analysis was inconsistent with the eventual diagnosis. Physicians shouldn’t solely rely on peritoneal fluid analysis, but also take into account the patient’s history when narrowing their differential.
Disclosures:
Nikhil Furtado, BS1, Suhail Sidhu, BS1, Thomas Checketts, DO1, Syed Mohsin Saghir, MD2, Rajani Rangray, MBBS1. P2474 - Cardiac Ascites With an Unusual Presentation on Peritoneal Fluid Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Creighton University School of Medicine, Omaha, NE; 2Creighton University, Omaha, NE
Introduction: Ascites is a pathological process of fluid accumulation in the peritoneal cavity predominantly secondary to cirrhosis, cancer, or heart failure. Peritoneal fluid analysis is an effective way to narrow the differential for new onset ascites by analyzing cell count and differential, albumin, total protein, and serum ascites albumin gradient (SAAG). Here we present a case where the typical diagnostic criteria for peritoneal fluid was inconsistent with the correct etiology.
Case Description/Methods: A 37-year-old man with past medical history of bronchopulmonary dysplasia, chronic respiratory failure on supplemental oxygen, pulmonary hypertension, right-sided HFpEF, hypertension, hyperlipidemia, and obesity presented with a congestive heart failure exacerbation. He reported worsening dyspnea, orthopnea, and peripheral edema for weeks. Physical exam revealed diminished breath sounds, tachycardia, abdominal distension, and 2 + lower extremity edema. Vitals included: T: 36.5 °C (97.7 °F), BP: 142/84, HR: 93, and SpO2: 95%. Given the abdominal distension, ascites was a concern. Paracentesis revealed 947 polymorphonuclear neutrophils (PMNs), which is diagnostic for spontaneous bacterial peritonitis, commonly occurring in cirrhosis. Cultures were negative. He was started on ceftriaxone then escalated to Zosyn due to increasing PMNs. SAAG was < 1.1 g/dl, suggesting ascites wasn’t due to portal hypertension, making heart failure and cirrhosis less likely. Ascites total protein and B-type natriuretic peptide were elevated at 4.5 g/dl and 6,548 pg/ml, respectively, consistent with heart failure. However, abdominal CT suggested cirrhosis, further confusing the picture. Cross-sectional imaging was negative for malignancy. He was discharged after his dyspnea, edema, and PMNs improved with intravenous furosemide and Zosyn. During outpatient follow-up with gastroenterology, a transjugular liver biopsy revealed normal histology with hepatic vein pressure gradient of 1 mmHg, excluding cirrhosis. Therefore, despite SAAG < 1.1 g/dl, it was deemed the ascites was secondary to the patient’s right-sided heart failure.
Discussion: While peritoneal fluid analysis is the preferred method to work-up new onset ascites, it is not always accurate. In this case, our patient's fluid analysis was inconsistent with the eventual diagnosis. Physicians shouldn’t solely rely on peritoneal fluid analysis, but also take into account the patient’s history when narrowing their differential.
Disclosures:
Nikhil Furtado indicated no relevant financial relationships.
Suhail Sidhu indicated no relevant financial relationships.
Thomas Checketts indicated no relevant financial relationships.
Syed Mohsin Saghir indicated no relevant financial relationships.
Rajani Rangray indicated no relevant financial relationships.
Nikhil Furtado, BS1, Suhail Sidhu, BS1, Thomas Checketts, DO1, Syed Mohsin Saghir, MD2, Rajani Rangray, MBBS1. P2474 - Cardiac Ascites With an Unusual Presentation on Peritoneal Fluid Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
