Monday Poster Session
Category: Liver
P2476 - Syphilitic Hepatitis: A Rare Manifestation of Secondary Syphilis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AB
Arouj Bajwa, MD
St. Luke's University Hospital
Bethlehem, PA
Presenting Author(s)
Arouj Bajwa, MD, Ashley Tran, MD, Li Ge, MD, Jessica Fenner, PA-C
St. Luke's University Hospital, Bethlehem, PA
Introduction: Syphilis is caused by the spirochete Treponema pallidium and can involve multiple organs with diverse and often subtle clinical manifestations. Syphilitic hepatitis (SH) is rare with reported incidence of 0.2% to 3% in patients with secondary syphilis. We describe a case of SH in a young woman with mixed liver injury.
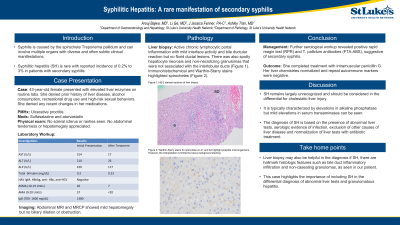
Case Description/Methods: 43-year-old female with history of ulcerative proctitis presented with elevated liver enzymes on routine labs. Her medications included sulfasalazine and atorvastatin. She denied prior history of liver disease, alcohol consumption, recreational drug use and high-risk sexual behaviors. She denied any recent changes in her medications. Physical exam was unremarkable. Labs revealed alkaline phosphatase 220 U/L, ALT 210 U/L, AST 154 U/L, and total bilirubin 0.3 mg/dL. Viral serologies were negative for hepatitis A, B, and C as well as HIV. Additional workup revealed mildly positive anti-mitochondrial and anti-smooth muscle antibodies but normal immunoglobulins. Abdominal MRI and MRCP showed mild hepatomegaly but no biliary dilation or obstruction. She had a percutaneous liver biopsy which showed active chronic lymphocytic portal inflammation with mild interface activity and bile ductular reaction but no florid ductal lesions. There was also spotty hepatocyte necrosis and non-necrotizing granulomas that were not associated with the interlobular ducts. Immunohistochemical and Warthin-Starry stains highlighted spirochetes. Further serological workup revealed positive rapid reagin test (RPR) and T. pallidum antibodies (FTA-ABS), suggestive of secondary syphilis. She completed treatment with intramuscular penicillin G with improvement of her liver chemistries.
Discussion: SH remains largely unrecognized and should be considered in the differential for cholestatic liver injury. It is typically characterized by elevations in alkaline phosphatase but mild elevations in serum transaminases can be seen. The diagnosis of SH is based on the presence of abnormal liver tests, serologic evidence of infection, exclusion of other causes of liver disease and normalization of liver tests with antibiotic treatment. However, liver biopsy may also be helpful in the diagnosis if there are hallmark histologic features such as bile duct inflammatory infiltration and non-caseating granulomas, as seen in our patient. This case highlights the importance of including SH in the differential diagnosis of abnormal liver tests and granulomatous hepatitis.

Disclosures:
Arouj Bajwa, MD, Ashley Tran, MD, Li Ge, MD, Jessica Fenner, PA-C. P2476 - Syphilitic Hepatitis: A Rare Manifestation of Secondary Syphilis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
St. Luke's University Hospital, Bethlehem, PA
Introduction: Syphilis is caused by the spirochete Treponema pallidium and can involve multiple organs with diverse and often subtle clinical manifestations. Syphilitic hepatitis (SH) is rare with reported incidence of 0.2% to 3% in patients with secondary syphilis. We describe a case of SH in a young woman with mixed liver injury.
Case Description/Methods: 43-year-old female with history of ulcerative proctitis presented with elevated liver enzymes on routine labs. Her medications included sulfasalazine and atorvastatin. She denied prior history of liver disease, alcohol consumption, recreational drug use and high-risk sexual behaviors. She denied any recent changes in her medications. Physical exam was unremarkable. Labs revealed alkaline phosphatase 220 U/L, ALT 210 U/L, AST 154 U/L, and total bilirubin 0.3 mg/dL. Viral serologies were negative for hepatitis A, B, and C as well as HIV. Additional workup revealed mildly positive anti-mitochondrial and anti-smooth muscle antibodies but normal immunoglobulins. Abdominal MRI and MRCP showed mild hepatomegaly but no biliary dilation or obstruction. She had a percutaneous liver biopsy which showed active chronic lymphocytic portal inflammation with mild interface activity and bile ductular reaction but no florid ductal lesions. There was also spotty hepatocyte necrosis and non-necrotizing granulomas that were not associated with the interlobular ducts. Immunohistochemical and Warthin-Starry stains highlighted spirochetes. Further serological workup revealed positive rapid reagin test (RPR) and T. pallidum antibodies (FTA-ABS), suggestive of secondary syphilis. She completed treatment with intramuscular penicillin G with improvement of her liver chemistries.
Discussion: SH remains largely unrecognized and should be considered in the differential for cholestatic liver injury. It is typically characterized by elevations in alkaline phosphatase but mild elevations in serum transaminases can be seen. The diagnosis of SH is based on the presence of abnormal liver tests, serologic evidence of infection, exclusion of other causes of liver disease and normalization of liver tests with antibiotic treatment. However, liver biopsy may also be helpful in the diagnosis if there are hallmark histologic features such as bile duct inflammatory infiltration and non-caseating granulomas, as seen in our patient. This case highlights the importance of including SH in the differential diagnosis of abnormal liver tests and granulomatous hepatitis.

Figure: Non-necrotizing granuloma (G) is present and not associated with interlobular bile duct (BD).
Disclosures:
Arouj Bajwa indicated no relevant financial relationships.
Ashley Tran indicated no relevant financial relationships.
Li Ge indicated no relevant financial relationships.
Jessica Fenner indicated no relevant financial relationships.
Arouj Bajwa, MD, Ashley Tran, MD, Li Ge, MD, Jessica Fenner, PA-C. P2476 - Syphilitic Hepatitis: A Rare Manifestation of Secondary Syphilis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
