Monday Poster Session
Category: Liver
P2480 - Acute Liver Failure With Liver Enzymes >5,000 in Sickle Cell Disease
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- NW
Neha Wadhavkar, MD
Brown University
Providence, Rhode Island
Presenting Author(s)
Neha Wadhavkar, MD, John Paul Nsubuga, MD, Nouran Ibrahim, BA, Prasanna Kumar, MD, Andrew Hsu, MD, Shannon Simmons, MD
Brown University, Providence, RI
Introduction: Sickle cell disease (SCD) is a hemoglobinopathy often complicated by painful vaso-occlusive episodes, acute chest syndrome, stroke, and myocardial infarction, affecting over 100,000 people in the United States. Sickle cell intrahepatic cholestasis (SCIC) is a rare and potentially fatal complication of SCD. Cases of SCIC have been sparsely documented across current literature. SCIC is thought to involve progressive hepatic injury due to sickling of hemoglobin within the sinusoids. To date, there is no consensus on appropriate management of SCIC, which can include supportive care, simple transfusion, red blood cell exchange transfusion, or liver transplant. We aim to highlight the importance of early recognition and evaluate the efficacy of various management approaches.
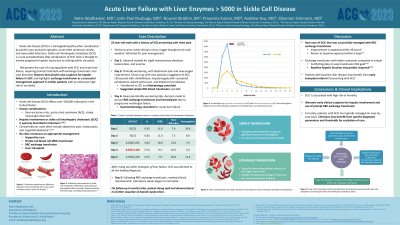
Case Description/Methods: A 32-year-old male with a history of SCD presented with severe chest pain. He developed hypoxia and new opacities on chest x-ray imaging suggestive of acute chest syndrome. Simultaneously, he developed abdominal pain, marked transaminase elevation (AST 6188, ALT 2501), acute kidney injury, and leukocytosis, suggesting SCIC with worsening hemolysis and multiorgan involvement. FFP, simple transfusion, and NAC were administered with no improvement. Hepatic and renal function continued to worsen (AST 8503, ALT 3340, Cr 5.74), prompting decision to treat with exchange transfusion and emergent dialysis. Following transfusion, hepatic function and overall clinical status dramatically improved (AST 3190, ALT 2410). On follow-up 6 months later, no sequelae of hepatic dysfunction were noted.
Discussion: Our case describes features of acute liver failure in SCIC and highlights exchange transfusion as a successful management approach in similar patients with an otherwise high risk of mortality. Clinical suspicion should be high when hyperbilirubinemia, rapidly rising transaminases, and multiorgan failure are present. In our patient, there was no clinical response to simple transfusion. Following exchange transfusion, marked improvement in hepatic function occurred within 24 hours, consistent with other case studies encouraging consideration of exchange transfusion as routine management for acute liver failure in SCIC. Normal baseline hepatic function seems to be a critical predictor of responsiveness to exchange transfusion and may guide escalation-of-care decisions, such as early transplant referral in older patients with underlying liver disease.

Disclosures:
Neha Wadhavkar, MD, John Paul Nsubuga, MD, Nouran Ibrahim, BA, Prasanna Kumar, MD, Andrew Hsu, MD, Shannon Simmons, MD. P2480 - Acute Liver Failure With Liver Enzymes >5,000 in Sickle Cell Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Brown University, Providence, RI
Introduction: Sickle cell disease (SCD) is a hemoglobinopathy often complicated by painful vaso-occlusive episodes, acute chest syndrome, stroke, and myocardial infarction, affecting over 100,000 people in the United States. Sickle cell intrahepatic cholestasis (SCIC) is a rare and potentially fatal complication of SCD. Cases of SCIC have been sparsely documented across current literature. SCIC is thought to involve progressive hepatic injury due to sickling of hemoglobin within the sinusoids. To date, there is no consensus on appropriate management of SCIC, which can include supportive care, simple transfusion, red blood cell exchange transfusion, or liver transplant. We aim to highlight the importance of early recognition and evaluate the efficacy of various management approaches.
Case Description/Methods: A 32-year-old male with a history of SCD presented with severe chest pain. He developed hypoxia and new opacities on chest x-ray imaging suggestive of acute chest syndrome. Simultaneously, he developed abdominal pain, marked transaminase elevation (AST 6188, ALT 2501), acute kidney injury, and leukocytosis, suggesting SCIC with worsening hemolysis and multiorgan involvement. FFP, simple transfusion, and NAC were administered with no improvement. Hepatic and renal function continued to worsen (AST 8503, ALT 3340, Cr 5.74), prompting decision to treat with exchange transfusion and emergent dialysis. Following transfusion, hepatic function and overall clinical status dramatically improved (AST 3190, ALT 2410). On follow-up 6 months later, no sequelae of hepatic dysfunction were noted.
Discussion: Our case describes features of acute liver failure in SCIC and highlights exchange transfusion as a successful management approach in similar patients with an otherwise high risk of mortality. Clinical suspicion should be high when hyperbilirubinemia, rapidly rising transaminases, and multiorgan failure are present. In our patient, there was no clinical response to simple transfusion. Following exchange transfusion, marked improvement in hepatic function occurred within 24 hours, consistent with other case studies encouraging consideration of exchange transfusion as routine management for acute liver failure in SCIC. Normal baseline hepatic function seems to be a critical predictor of responsiveness to exchange transfusion and may guide escalation-of-care decisions, such as early transplant referral in older patients with underlying liver disease.

Figure: Figure 1. Visualization of aspartate transaminase (AST) and alanine transaminase (ALT) trend throughout hospital course with exchange transfusion on hospital day 4, as indicated by arrow.
Disclosures:
Neha Wadhavkar indicated no relevant financial relationships.
John Paul Nsubuga indicated no relevant financial relationships.
Nouran Ibrahim indicated no relevant financial relationships.
Prasanna Kumar indicated no relevant financial relationships.
Andrew Hsu indicated no relevant financial relationships.
Shannon Simmons indicated no relevant financial relationships.
Neha Wadhavkar, MD, John Paul Nsubuga, MD, Nouran Ibrahim, BA, Prasanna Kumar, MD, Andrew Hsu, MD, Shannon Simmons, MD. P2480 - Acute Liver Failure With Liver Enzymes >5,000 in Sickle Cell Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
