Monday Poster Session
Category: Liver
P2482 - Rare Case of Hepatic Amyloidosis in a Patient With Recurrent Ascites
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- HS
Harjit Singh, MD
MedStar Georgetown University Hospital
Washington, District of Columbia
Presenting Author(s)
Harjit Singh, MD, Sherry Gholami, MD, Bryce Kunkle, MD, Roya Zarpak, MD, Amol S. Rangnekar, MD
MedStar Georgetown University Hospital, Washington, DC
Introduction: Hepatic amyloidosis is a rare cause of ascites in patients and diagnosis and management are difficult. Herein, we present a case of hepatic amyloidosis in a patient who presented with recurrent ascites.
Case Description/Methods: 70-year-old male with past medical history of ESRD secondary to amyloidosis presented to clinic after recent hospitalization for hemorrhagic shock with complaints of recurrent worsening abdominal distention and pruritis. For his amyloidosis, he had been previously treated with melphalan and undergone autologous bone marrow transplantation.
On examination, vitals were within normal limits, and his abdomen was mildly distended. During his hospitalization, he had undergone imaging which demonstrated ascites, hemoperitoneum, and atraumatic splenic rupture. He underwent diagnostic paracentesis which showed evidence of hemorrhagic ascites. Hepatic venous pressure gradient was 1 mmHg, and no other evidence of cirrhosis was noted on imaging. Serologic testing was negative for other liver diseases. Cardiac etiologies of his ascites had also been ruled out. Finally, he underwent transjugular liver biopsy which identified marked sinusoidal dilation and positive Congo Red staining consistent with hepatic amyloidosis (Figure 1). Given the clinical, imaging, and pathological findings, the patient was diagnosed with hepatic amyloidosis.
Thereafter, the patient had been managing his symptoms through recurrent paracentesis. Unfortunately, he had recurrence of hemorrhagic shock and passed away from associated complications.
Discussion: Hepatic amyloidosis is an uncommon cause of ascites, but one that should be of concern in a patient with recurrent unexplained ascites. Diagnosis is difficult as patients present nonspecifically with abdominal distention, fatigue, and hepatomegaly. Amyloid deposition occurs either within the sinuses or the liver parenchyma itself. Imaging is often nonspecific and definitive diagnosis occurs with liver biopsy and subsequent pathological analysis. Treatment options are limited and aimed at symptom management. A subset of patients may be treated with the chemotherapeutic agent melphalan; however, outcomes are poor. Most patients have a limited prognosis and death occurs within a year.

Disclosures:
Harjit Singh, MD, Sherry Gholami, MD, Bryce Kunkle, MD, Roya Zarpak, MD, Amol S. Rangnekar, MD. P2482 - Rare Case of Hepatic Amyloidosis in a Patient With Recurrent Ascites, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
MedStar Georgetown University Hospital, Washington, DC
Introduction: Hepatic amyloidosis is a rare cause of ascites in patients and diagnosis and management are difficult. Herein, we present a case of hepatic amyloidosis in a patient who presented with recurrent ascites.
Case Description/Methods: 70-year-old male with past medical history of ESRD secondary to amyloidosis presented to clinic after recent hospitalization for hemorrhagic shock with complaints of recurrent worsening abdominal distention and pruritis. For his amyloidosis, he had been previously treated with melphalan and undergone autologous bone marrow transplantation.
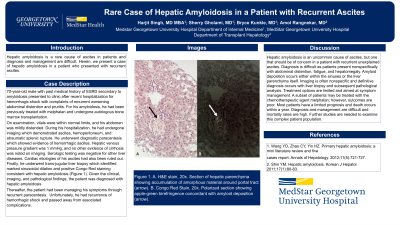
On examination, vitals were within normal limits, and his abdomen was mildly distended. During his hospitalization, he had undergone imaging which demonstrated ascites, hemoperitoneum, and atraumatic splenic rupture. He underwent diagnostic paracentesis which showed evidence of hemorrhagic ascites. Hepatic venous pressure gradient was 1 mmHg, and no other evidence of cirrhosis was noted on imaging. Serologic testing was negative for other liver diseases. Cardiac etiologies of his ascites had also been ruled out. Finally, he underwent transjugular liver biopsy which identified marked sinusoidal dilation and positive Congo Red staining consistent with hepatic amyloidosis (Figure 1). Given the clinical, imaging, and pathological findings, the patient was diagnosed with hepatic amyloidosis.
Thereafter, the patient had been managing his symptoms through recurrent paracentesis. Unfortunately, he had recurrence of hemorrhagic shock and passed away from associated complications.
Discussion: Hepatic amyloidosis is an uncommon cause of ascites, but one that should be of concern in a patient with recurrent unexplained ascites. Diagnosis is difficult as patients present nonspecifically with abdominal distention, fatigue, and hepatomegaly. Amyloid deposition occurs either within the sinuses or the liver parenchyma itself. Imaging is often nonspecific and definitive diagnosis occurs with liver biopsy and subsequent pathological analysis. Treatment options are limited and aimed at symptom management. A subset of patients may be treated with the chemotherapeutic agent melphalan; however, outcomes are poor. Most patients have a limited prognosis and death occurs within a year.

Figure: Figure 1. A. H&E stain, 20x. Section of hepatic parenchyma showing accumulation of amorphous material around portal tract (arrow). B. Congo Red Stain, 20x. Polarized section showing apple-green birefringence concordant with amyloid deposition (arrow).
Disclosures:
Harjit Singh indicated no relevant financial relationships.
Sherry Gholami indicated no relevant financial relationships.
Bryce Kunkle indicated no relevant financial relationships.
Roya Zarpak indicated no relevant financial relationships.
Amol Rangnekar indicated no relevant financial relationships.
Harjit Singh, MD, Sherry Gholami, MD, Bryce Kunkle, MD, Roya Zarpak, MD, Amol S. Rangnekar, MD. P2482 - Rare Case of Hepatic Amyloidosis in a Patient With Recurrent Ascites, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
