Monday Poster Session
Category: Liver
P2493 - Hepatic Arteriosclerosis: A Rare Microvascular Complication of Diabetes
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Joy-Marie Hermes, MD
Scripps Clinic
La Jolla, CA
Presenting Author(s)
Joy-Marie Hermes, MD, Fei Bao, MD, Adam Deising, MD
Scripps Clinic, La Jolla, CA
Introduction: Diabetes is associated with an increased risk of chronic liver disease. Classically, this includes non-alcoholic steatohepatitis (NASH) and glycogenic hepatopathy. Microvascular hepatic complications are rarely diagnosed in clinical practice, especially in the absence of liver biopsy. This case highlights hepatic arteriosclerosis (HA), an infrequently encountered complication of long-standing poor glycemic control.
Case Description/Methods: A 49 year old female with a history of Roux-en-Y gastric bypass, type 1 diabetes mellitus and hypertension was referred for evaluation of abnormal liver enzymes. She had evidence of mild AST and ALT elevation (ranging from 16-130) dating back 5 years. Chronically, she had poor glycemic control with hemoglobin A1c measured up to 13%. She denied any alcohol, herbal or dietary supplement use or family history of liver disease. Abdominal ultrasound and laboratory workup including hepatitis serologies and antibody testing was unremarkable. FibroScan demonstrated a median score of 8.8 kPa and CAP 198 dB/m, consistent with F1/F2 fibrosis and no steatosis.
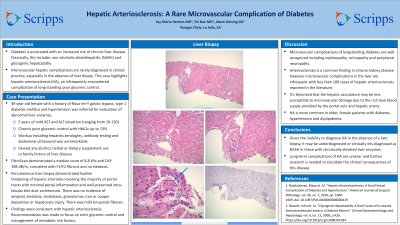
Percutaneous liver biopsy demonstrated hyaline thickening of hepatic arterioles involving the majority of portal tracts with minimal portal inflammation and well-preserved intra-lobular bile duct architecture. There was no evidence of amyloid, steatosis, cholestasis, granulomas, iron or copper deposition or hepatocyte injury. There was mild sinusoidal fibrosis. Findings were consistent with hepatic arteriosclerosis. The recommendation was made to focus on strict glycemic control and management of metabolic risk factors.
Discussion: Microvascular complications of longstanding diabetes are well-recognized including nephropathy, retinopathy and peripheral neuropathy. Arteriosclerosis is a common finding in chronic kidney disease however microvascular complications in the liver are infrequent with less than 100 cases of HA reported in the literature. It is thought that the hepatic vasculature may be less susceptible to microvascular damage due to the rich dual blood supply provided by the portal vein and hepatic artery. HA is more likely in older, female patients with diabetes, hypertension and dyslipidemia. Given the inability to diagnose HA in the absence of a liver biopsy, it may be underdiagnosed or clinically mis-diagnosed as NASH in those with chronically elevated liver enzymes. Long-term complications of HA are unclear and further research is needed to elucidate the clinical consequences of this disease.

Disclosures:
Joy-Marie Hermes, MD, Fei Bao, MD, Adam Deising, MD. P2493 - Hepatic Arteriosclerosis: A Rare Microvascular Complication of Diabetes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Scripps Clinic, La Jolla, CA
Introduction: Diabetes is associated with an increased risk of chronic liver disease. Classically, this includes non-alcoholic steatohepatitis (NASH) and glycogenic hepatopathy. Microvascular hepatic complications are rarely diagnosed in clinical practice, especially in the absence of liver biopsy. This case highlights hepatic arteriosclerosis (HA), an infrequently encountered complication of long-standing poor glycemic control.
Case Description/Methods: A 49 year old female with a history of Roux-en-Y gastric bypass, type 1 diabetes mellitus and hypertension was referred for evaluation of abnormal liver enzymes. She had evidence of mild AST and ALT elevation (ranging from 16-130) dating back 5 years. Chronically, she had poor glycemic control with hemoglobin A1c measured up to 13%. She denied any alcohol, herbal or dietary supplement use or family history of liver disease. Abdominal ultrasound and laboratory workup including hepatitis serologies and antibody testing was unremarkable. FibroScan demonstrated a median score of 8.8 kPa and CAP 198 dB/m, consistent with F1/F2 fibrosis and no steatosis.
Percutaneous liver biopsy demonstrated hyaline thickening of hepatic arterioles involving the majority of portal tracts with minimal portal inflammation and well-preserved intra-lobular bile duct architecture. There was no evidence of amyloid, steatosis, cholestasis, granulomas, iron or copper deposition or hepatocyte injury. There was mild sinusoidal fibrosis. Findings were consistent with hepatic arteriosclerosis. The recommendation was made to focus on strict glycemic control and management of metabolic risk factors.
Discussion: Microvascular complications of longstanding diabetes are well-recognized including nephropathy, retinopathy and peripheral neuropathy. Arteriosclerosis is a common finding in chronic kidney disease however microvascular complications in the liver are infrequent with less than 100 cases of HA reported in the literature. It is thought that the hepatic vasculature may be less susceptible to microvascular damage due to the rich dual blood supply provided by the portal vein and hepatic artery. HA is more likely in older, female patients with diabetes, hypertension and dyslipidemia. Given the inability to diagnose HA in the absence of a liver biopsy, it may be underdiagnosed or clinically mis-diagnosed as NASH in those with chronically elevated liver enzymes. Long-term complications of HA are unclear and further research is needed to elucidate the clinical consequences of this disease.

Figure: Liver biopsy
Disclosures:
Joy-Marie Hermes indicated no relevant financial relationships.
Fei Bao indicated no relevant financial relationships.
Adam Deising indicated no relevant financial relationships.
Joy-Marie Hermes, MD, Fei Bao, MD, Adam Deising, MD. P2493 - Hepatic Arteriosclerosis: A Rare Microvascular Complication of Diabetes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
