Monday Poster Session
Category: Liver
P2540 - DILI - Gently Differentiating Autoimmune Liver Diseases
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- MA
Mohammed S. Al-Zakwani, MD, MS
UT Health San Antonio
San Antonio, TX
Presenting Author(s)
Mohammed S. Al-Zakwani, MD, MS1, Umesha Boregowda, MD1, Jacob Ritter, MD1, Lisa Pedicone, PhD2, Carmen Landaverde, MD3, Eric Lawitz, MD3, Jan Petrasek, MD, PhD4, Fred Poordad, MD3, Fabian Rodas, MD3, Eugenia Tsai, MD3
1UT Health San Antonio, San Antonio, TX; 2Texas Liver Institute, San Antonio, TX; 3UT Health San Antonio, Texas Liver Institute, San Antonio, TX; 4UT Health San Antonio, Texas Liver Institute, Jackson, MS
Introduction: Drug-induced autoimmune liver disease (DI-AILD) is an entity that is distinct from idiopathic autoimmune hepatitis (AIH). Here we present a rare case of a patient experiencing DI-AILD secondary to statin use.
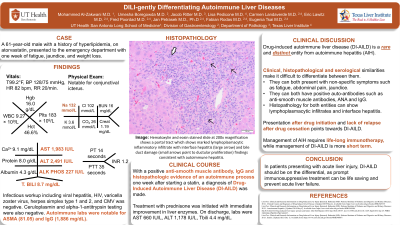
Case Description/Methods: A 61-year-old male with a history of hyperlipidemia, on atorvastatin presented to the emergency department with one week of fatigue, jaundice, and weight loss. The patient returned from a five-month stay in Mexico during which he purchased over-the-counter (OTC) atorvastatin. He was hemodynamically stable, with a physical exam notable for conjunctival icterus. Lab workup demonstrated AST 1,983 IU/L, ALT 2,491 IU/L, ALP 227 IU/L, Tbili 8.7 mg/dL, INR 1.2. Infectious workup including viral hepatitis, HIV, varicella zoster virus, herpes simplex type 1 and 2, and CMV was negative. Autoimmune labs were notable for ASMA (81.05) and IgG (1,886 mg/dL). Rousel Uclaf Causality Assessment Method score was 8, suggesting probable drug-induced liver injury (DILI). MRI/MRCP showed normal liver and no evidence of biliary obstruction. Liver biopsy demonstrated portal and lobular lymphoplasmacytic infiltrates with interface hepatitis, suggestive of an autoimmune process (Figure 1). Treatment with prednisone was initiated with immediate improvement in liver enzymes. On discharge, labs were AST 660 IU/L, ALT 1,178 IU/L, Tbili 4.4 mg/dL, and INR 1.0.
Discussion: Various drugs, including statins, may cause DILI. However, DI-AILD is less common. Although DI-AILD and AIH have clinical, serological, and histopathological similarities, differentiating them is important as it changes clinical management. Obtaining a thorough clinical history is crucial as timing of drug initiation in relation to clinical presentation can aid in an accurate diagnosis. Resolution of the syndrome upon withdrawal of the suspected drug and lack of relapse with withdrawal of immunomodulatory therapy is suggestive of DI-AILD. Idiopathic AIH usually requires lifelong immunosuppression, while management of DI-AILD tends to be more short-term.
While clinically, it may be difficult to distinguish between AIH and DI-AILD, the timing one week after starting OTC statin is suggestive of DI-AILD. This case highlights the importance of not only maintaining a high level of clinical suspicion for DILI in patients with acutely elevated liver tests but also including DI-AILD as part of the differential. Early recognition and prompt immunosuppressive treatment can prevent acute liver failure and reduce morbidity.

Disclosures:
Mohammed S. Al-Zakwani, MD, MS1, Umesha Boregowda, MD1, Jacob Ritter, MD1, Lisa Pedicone, PhD2, Carmen Landaverde, MD3, Eric Lawitz, MD3, Jan Petrasek, MD, PhD4, Fred Poordad, MD3, Fabian Rodas, MD3, Eugenia Tsai, MD3. P2540 - DILI - Gently Differentiating Autoimmune Liver Diseases, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UT Health San Antonio, San Antonio, TX; 2Texas Liver Institute, San Antonio, TX; 3UT Health San Antonio, Texas Liver Institute, San Antonio, TX; 4UT Health San Antonio, Texas Liver Institute, Jackson, MS
Introduction: Drug-induced autoimmune liver disease (DI-AILD) is an entity that is distinct from idiopathic autoimmune hepatitis (AIH). Here we present a rare case of a patient experiencing DI-AILD secondary to statin use.
Case Description/Methods: A 61-year-old male with a history of hyperlipidemia, on atorvastatin presented to the emergency department with one week of fatigue, jaundice, and weight loss. The patient returned from a five-month stay in Mexico during which he purchased over-the-counter (OTC) atorvastatin. He was hemodynamically stable, with a physical exam notable for conjunctival icterus. Lab workup demonstrated AST 1,983 IU/L, ALT 2,491 IU/L, ALP 227 IU/L, Tbili 8.7 mg/dL, INR 1.2. Infectious workup including viral hepatitis, HIV, varicella zoster virus, herpes simplex type 1 and 2, and CMV was negative. Autoimmune labs were notable for ASMA (81.05) and IgG (1,886 mg/dL). Rousel Uclaf Causality Assessment Method score was 8, suggesting probable drug-induced liver injury (DILI). MRI/MRCP showed normal liver and no evidence of biliary obstruction. Liver biopsy demonstrated portal and lobular lymphoplasmacytic infiltrates with interface hepatitis, suggestive of an autoimmune process (Figure 1). Treatment with prednisone was initiated with immediate improvement in liver enzymes. On discharge, labs were AST 660 IU/L, ALT 1,178 IU/L, Tbili 4.4 mg/dL, and INR 1.0.
Discussion: Various drugs, including statins, may cause DILI. However, DI-AILD is less common. Although DI-AILD and AIH have clinical, serological, and histopathological similarities, differentiating them is important as it changes clinical management. Obtaining a thorough clinical history is crucial as timing of drug initiation in relation to clinical presentation can aid in an accurate diagnosis. Resolution of the syndrome upon withdrawal of the suspected drug and lack of relapse with withdrawal of immunomodulatory therapy is suggestive of DI-AILD. Idiopathic AIH usually requires lifelong immunosuppression, while management of DI-AILD tends to be more short-term.
While clinically, it may be difficult to distinguish between AIH and DI-AILD, the timing one week after starting OTC statin is suggestive of DI-AILD. This case highlights the importance of not only maintaining a high level of clinical suspicion for DILI in patients with acutely elevated liver tests but also including DI-AILD as part of the differential. Early recognition and prompt immunosuppressive treatment can prevent acute liver failure and reduce morbidity.

Figure: Figure 1. Histology from liver biopsy demonstrates portal tracts with marked lymphoplasmacytic inflammatory infiltrate and interface hepatitis (white arrow) and bile duct damage with ductular proliferation (black arrows), findings suggestive of an autoimmune process. Hematoxylin and eosin stain, 200x.
Disclosures:
Mohammed Al-Zakwani indicated no relevant financial relationships.
Umesha Boregowda indicated no relevant financial relationships.
Jacob Ritter indicated no relevant financial relationships.
Lisa Pedicone indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Eric Lawitz: 89Bio, Inc – Grant/Research Support. AbbVie – Grant/Research Support, Speakers Bureau. Akero – Advisor or Review Panel Member, Grant/Research Support. Allergan – Grant/Research Support. Alnylam – Grant/Research Support. Amgen – Grant/Research Support. Ascelia Pharma – Grant/Research Support. AstraZeneca – Grant/Research Support. Axcella Health – Grant/Research Support. Boehringer Ingelheim – Advisor or Review Panel Member, Grant/Research Support. Bristol Myers Squibb – Advisor or Review Panel Member, Grant/Research Support. Conatus Pharmaceuticals – Grant/Research Support. Cymabay – Grant/Research Support. CytoDyn – Grant/Research Support. DSM – Grant/Research Support. Durect Corporation – Grant/Research Support. Gilead – Speakers Bureau. Intercept – Advisor or Review Panel Member, Grant/Research Support, Speakers Bureau. Metacrine – Advisor or Review Panel Member. Novo Nordisk – Advisor or Review Panel Member. Sagimet – Advisor or Review Panel Member. Terns – Advisor or Review Panel Member.
Jan Petrasek indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Mohammed S. Al-Zakwani, MD, MS1, Umesha Boregowda, MD1, Jacob Ritter, MD1, Lisa Pedicone, PhD2, Carmen Landaverde, MD3, Eric Lawitz, MD3, Jan Petrasek, MD, PhD4, Fred Poordad, MD3, Fabian Rodas, MD3, Eugenia Tsai, MD3. P2540 - DILI - Gently Differentiating Autoimmune Liver Diseases, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
