Monday Poster Session
Category: Liver
P2546 - Single-Culprit Pyogenic Liver Abscess Diagnosed by CT-Guided Percutaneous Aspiration: A Case Review
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AP
Aaron Perez, DO
Larkin Community Hospital
South Miami, FL
Presenting Author(s)
Aaron Perez, DO1, Paul A. Felix Lopez, 2, Kamal Akbar, MD1, Martha Arevalo-Mora, MD1, Natalia Martin, DO1
1Larkin Community Hospital, South Miami, FL; 2University of Medicine and Health Sciences, St. Kitts, Saint George Basseterre, Saint Kitts and Nevis
Introduction: Pyogenic liver abscesses are the most common type of abdominal organ abscess with an annual incidence 2.3 to 17.6 cases per 100,000 population. This infection often arises in the setting of biliary disruption. Although most cases are classically polymicrobial enteric flora infections, we report a case due to a single culprit, Serratia marcescens. Due to the limited number of reported cases, this case review article aims to update on the diagnosis and management of this rarely described entity.
Case Description/Methods: A 32-year-old male cruise line worker from Bali presented to our Emergency Department with a 10-day history of non-productive cough. Onboard evaluation CXR showed diaphragmatic asymmetry prompting further workup. Abdominal CT depicted a 10 cm diameter right lobe hepatic multiseptated complex cystic mass with peripheral rim enhancement. Abscess formation was confirmed with a triple-phase CT. Lab work showed a 76 mg/dl ALT, a 378 mg/dl ALP, and thrombocytosis (649 k). CT-guided percutaneous aspiration of the liver lesion was performed. Culture grew Serratia marcescens. Empirical IV treatment with Metronidazole and Ceftriaxone was given. Abscess was managed with a JP drain, exhibiting a lesion reduction to 5.9 cm in diameter. The patient was discharged with oral antibiotic therapy and follow-up imaging.
Discussion: Risk factors for pyogenic abdominal abscesses include leukocyte immune dysfunction, underlying hepatopancreatobiliary disease, chronic PPI use, and residing in East Asia. A high degree of clinical suspicion is required in patients with nonspecific abdominal symptoms and/or fever of unknown origin. Workup usually shows elevated leukocytes, ALP, and bilirubin levels. Isolated transaminitis occur in 50%. Confirmatory diagnosis via CT or US-guided percutaneous aspiration with gram-stain and culture is required. In the US, most liver pyogenic abscesses are polymicrobial (Streptococcus milleri-group); liver abscess resulting from pure gram-positive cocci/co-infection with Candida spp. are rare. The Serratia sp. have been isolated in only 0.25% of pyogenic liver abscess cases. Thus, this single-entity pyogenic liver abscess case is a significant addition to literature. Despite Serratia marcescens infrequent presentation, this entity should be considered in the differential diagnosis. Standard of care management with antibiotic therapy and percutaneous drainage should ensue, yet EUS-guided drainage should be considered in difficult-to-access liver abscesses.

Disclosures:
Aaron Perez, DO1, Paul A. Felix Lopez, 2, Kamal Akbar, MD1, Martha Arevalo-Mora, MD1, Natalia Martin, DO1. P2546 - Single-Culprit Pyogenic Liver Abscess Diagnosed by CT-Guided Percutaneous Aspiration: A Case Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Larkin Community Hospital, South Miami, FL; 2University of Medicine and Health Sciences, St. Kitts, Saint George Basseterre, Saint Kitts and Nevis
Introduction: Pyogenic liver abscesses are the most common type of abdominal organ abscess with an annual incidence 2.3 to 17.6 cases per 100,000 population. This infection often arises in the setting of biliary disruption. Although most cases are classically polymicrobial enteric flora infections, we report a case due to a single culprit, Serratia marcescens. Due to the limited number of reported cases, this case review article aims to update on the diagnosis and management of this rarely described entity.
Case Description/Methods: A 32-year-old male cruise line worker from Bali presented to our Emergency Department with a 10-day history of non-productive cough. Onboard evaluation CXR showed diaphragmatic asymmetry prompting further workup. Abdominal CT depicted a 10 cm diameter right lobe hepatic multiseptated complex cystic mass with peripheral rim enhancement. Abscess formation was confirmed with a triple-phase CT. Lab work showed a 76 mg/dl ALT, a 378 mg/dl ALP, and thrombocytosis (649 k). CT-guided percutaneous aspiration of the liver lesion was performed. Culture grew Serratia marcescens. Empirical IV treatment with Metronidazole and Ceftriaxone was given. Abscess was managed with a JP drain, exhibiting a lesion reduction to 5.9 cm in diameter. The patient was discharged with oral antibiotic therapy and follow-up imaging.
Discussion: Risk factors for pyogenic abdominal abscesses include leukocyte immune dysfunction, underlying hepatopancreatobiliary disease, chronic PPI use, and residing in East Asia. A high degree of clinical suspicion is required in patients with nonspecific abdominal symptoms and/or fever of unknown origin. Workup usually shows elevated leukocytes, ALP, and bilirubin levels. Isolated transaminitis occur in 50%. Confirmatory diagnosis via CT or US-guided percutaneous aspiration with gram-stain and culture is required. In the US, most liver pyogenic abscesses are polymicrobial (Streptococcus milleri-group); liver abscess resulting from pure gram-positive cocci/co-infection with Candida spp. are rare. The Serratia sp. have been isolated in only 0.25% of pyogenic liver abscess cases. Thus, this single-entity pyogenic liver abscess case is a significant addition to literature. Despite Serratia marcescens infrequent presentation, this entity should be considered in the differential diagnosis. Standard of care management with antibiotic therapy and percutaneous drainage should ensue, yet EUS-guided drainage should be considered in difficult-to-access liver abscesses.

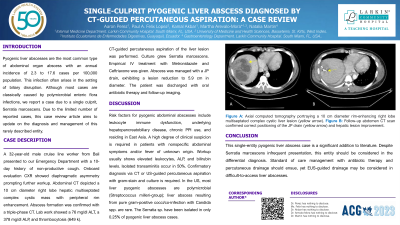
Figure: A. Axial computed tomography portraying a 10 cm diameter rim-enhancing right lobe multiseptated complex cystic liver lesion (yellow arrow).
B. Follow-up abdomen CT scan confirmed correct positioning of the JP drain (yellow arrow) and hepatic lesion improvement.
B. Follow-up abdomen CT scan confirmed correct positioning of the JP drain (yellow arrow) and hepatic lesion improvement.
Disclosures:
Aaron Perez indicated no relevant financial relationships.
Paul Felix Lopez indicated no relevant financial relationships.
Kamal Akbar indicated no relevant financial relationships.
Martha Arevalo-Mora indicated no relevant financial relationships.
Natalia Martin indicated no relevant financial relationships.
Aaron Perez, DO1, Paul A. Felix Lopez, 2, Kamal Akbar, MD1, Martha Arevalo-Mora, MD1, Natalia Martin, DO1. P2546 - Single-Culprit Pyogenic Liver Abscess Diagnosed by CT-Guided Percutaneous Aspiration: A Case Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
