Monday Poster Session
Category: Liver
P2552 - The Mimicker: A Case of Hepatic Inflammatory Pseudotumor
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Carla M. Cepero-Jimenez, MD
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Carla M. Cepero-Jimenez, MD, Reyshley Ramos-Marquez, MD, Henry De Jesus-de la Cruz, MD, Eduardo Acosta-Pumarejo, MD, Loscar Santiago-Rivera, MD, Doris H. Toro, MD, FACG
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Inflammatory pseudotumor (IPT) is a rare and benign tumor-like lesion of unclear etiology which is composed of fibrosis and inflammatory cell infiltrates. These lesions are most commonly found in the lung but can occur at other sites such as the liver. These hepatic lesions are usually solitary and localized at the right lobe. Liver IPTs occur most commonly in childhood and early adulthood. Imaging findings are inconclusive and frequently misinterpreted as malignant in nature. Liver biopsy is cardinal in establishing the diagnosis. Herein, we present a challenging case of an hepatic mass in a patient with history of 2 primary malignant neoplasms.
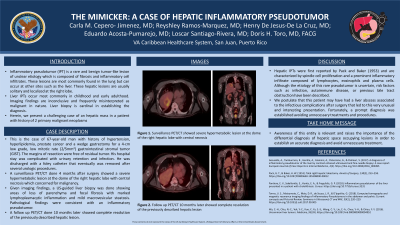
Case Description/Methods: This is the case of 67-year-old man with history of hypertension, hyperlipidemia, prostate cancer and a wedge gastrectomy for a 4-cm low grade, low mitotic rate (2/5mm2) gastrointestinal stromal tumor (GIST). The margins of resection were free of residual tumor. His hospital stay was complicated with urinary retention and infection. He was discharged with a foley catheter that eventually was removed after several urologic procedures. A surveillance PET/CT done 4 months after surgery showed a severe hypermetabolic lesion at the dome of the right hepatic lobe with central necrosis which concerned for malignancy. Given imaging findings, a US-guided liver biopsy was done showing areas of loss of parenchyma and focal fibrosis with marked lymphoplasmacytic inflammation and mild macrovesicular steatosis. Pathological findings were consistent with an inflammatory pseudotumor. A follow PET/CT done 10 months later showed complete resolution of the previously described hepatic lesion.
Discussion: Hepatic IPTs were first reported by Pack and Baker (1953) and are characterized by spindle cell proliferation and a prominent inflammatory infiltrate composed of lymphocytes, eosinophils and plasma cells. Although the etiology of this rare pseudotumor is uncertain, risk factors such as infection, autoimmune disease, or previous bile tract obstruction have been described. Awareness of this entity is relevant and raises the importance of the differential diagnosis of hepatic space occupying lesions in order to establish an accurate diagnosis and avoid unnecessary treatment. We postulate that this patient may have had a liver abscess associated to the infectious complications after surgery that led to this very unusual and interesting presentation. Fortunately, a prompt diagnosis was established avoiding unnecessary treatments and procedures.

Disclosures:
Carla M. Cepero-Jimenez, MD, Reyshley Ramos-Marquez, MD, Henry De Jesus-de la Cruz, MD, Eduardo Acosta-Pumarejo, MD, Loscar Santiago-Rivera, MD, Doris H. Toro, MD, FACG. P2552 - The Mimicker: A Case of Hepatic Inflammatory Pseudotumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Inflammatory pseudotumor (IPT) is a rare and benign tumor-like lesion of unclear etiology which is composed of fibrosis and inflammatory cell infiltrates. These lesions are most commonly found in the lung but can occur at other sites such as the liver. These hepatic lesions are usually solitary and localized at the right lobe. Liver IPTs occur most commonly in childhood and early adulthood. Imaging findings are inconclusive and frequently misinterpreted as malignant in nature. Liver biopsy is cardinal in establishing the diagnosis. Herein, we present a challenging case of an hepatic mass in a patient with history of 2 primary malignant neoplasms.
Case Description/Methods: This is the case of 67-year-old man with history of hypertension, hyperlipidemia, prostate cancer and a wedge gastrectomy for a 4-cm low grade, low mitotic rate (2/5mm2) gastrointestinal stromal tumor (GIST). The margins of resection were free of residual tumor. His hospital stay was complicated with urinary retention and infection. He was discharged with a foley catheter that eventually was removed after several urologic procedures. A surveillance PET/CT done 4 months after surgery showed a severe hypermetabolic lesion at the dome of the right hepatic lobe with central necrosis which concerned for malignancy. Given imaging findings, a US-guided liver biopsy was done showing areas of loss of parenchyma and focal fibrosis with marked lymphoplasmacytic inflammation and mild macrovesicular steatosis. Pathological findings were consistent with an inflammatory pseudotumor. A follow PET/CT done 10 months later showed complete resolution of the previously described hepatic lesion.
Discussion: Hepatic IPTs were first reported by Pack and Baker (1953) and are characterized by spindle cell proliferation and a prominent inflammatory infiltrate composed of lymphocytes, eosinophils and plasma cells. Although the etiology of this rare pseudotumor is uncertain, risk factors such as infection, autoimmune disease, or previous bile tract obstruction have been described. Awareness of this entity is relevant and raises the importance of the differential diagnosis of hepatic space occupying lesions in order to establish an accurate diagnosis and avoid unnecessary treatment. We postulate that this patient may have had a liver abscess associated to the infectious complications after surgery that led to this very unusual and interesting presentation. Fortunately, a prompt diagnosis was established avoiding unnecessary treatments and procedures.

Figure: Surveillance PET/CT showed severe hypermetabolic lesion at the dome of the right hepatic lobe with central necrosis (A and B). Follow up PET/CT 10 months later showed complete resolution of the previously described hepatic lesion (C and D).
Disclosures:
Carla Cepero-Jimenez indicated no relevant financial relationships.
Reyshley Ramos-Marquez indicated no relevant financial relationships.
Henry De Jesus-de la Cruz indicated no relevant financial relationships.
Eduardo Acosta-Pumarejo indicated no relevant financial relationships.
Loscar Santiago-Rivera indicated no relevant financial relationships.
Doris Toro indicated no relevant financial relationships.
Carla M. Cepero-Jimenez, MD, Reyshley Ramos-Marquez, MD, Henry De Jesus-de la Cruz, MD, Eduardo Acosta-Pumarejo, MD, Loscar Santiago-Rivera, MD, Doris H. Toro, MD, FACG. P2552 - The Mimicker: A Case of Hepatic Inflammatory Pseudotumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
