Monday Poster Session
Category: Liver
P2559 - Primary Sclerosing Cholangitis-Autoimmune Hepatitis Overlap Syndrome
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Muaaz Masood, MD
Virginia Mason Franciscan Health
Seattle, WA
Presenting Author(s)
Muaaz Masood, MD1, Asma Siddique, MD1, Rajesh Krishnamoorthi, MD1, Blaire Burman, MD1, Richard Kozarek, MD, FACG2
1Virginia Mason Franciscan Health, Seattle, WA; 2Virginia Mason Franciscan Health/Benaroya Research Institute, Seattle, WA
Introduction: Overlap syndromes with autoimmune hepatitis (AIH), primary sclerosing cholangitis (PSC) and primary biliary cirrhosis (PBC) may occur in 3-17% of patients with autoimmune liver disease. PSC-AIH is a rare entity which primarily affects young adults and involves biliary abnormalities of PSC in conjunction with features of AIH.
Case Description/Methods: A 29-year-old male with Crohn’s disease (CD) and biopsy-proven PSC who presented to the Hepatology clinic for persistently elevated liver enzymes. Recent ERCP revealed a mild stricture of the distal common bile duct which was dilated. Brushings were negative for abnormalities by fluorescence in situ hybridization. Repeat MRCP did not reveal biliary abnormalities. The patient reported fatigue, pruritus and dark urine, but denied fevers/chills, abdominal pain, change in bowel habits, weight loss, alcohol use, new medications or supplements. Vital signs were unremarkable. Examination revealed jaundice, scleral icterus and hepatomegaly. Laboratory studies were notable for AST 1091 U/L, ALT 892 U/L, AP 247 U/L, TB 14.1 mg/dL. Due to concern for overlap with AIH, further work-up was obtained which was notable for anti-nuclear antibody >1:640 in a homogeneous nuclear pattern, total IgG 2250 mg/dL, negative antimitochondrial antibody (AMA) and F-actin IgG >100 U. Repeat liver biopsy demonstrated moderate lymphoplasmacytic inflammation, interface activity, lobular necroinflammatory activity, stage II fibrosis – findings suggestive for superimposed AIH. He was started on steroids with resolution of his symptoms and liver enzyme abnormalities. The patient was subsequently switched to azathioprine with an excellent response. Mesalamine for CD was tapered and discontinued.
Discussion: PSC-AIH is considered to be a variant of AIH and is suspected with cholangiographic features of PSC, negative AMA and clinical, biochemical and histological evidence of AIH. No specific diagnostic criteria exist for PSC-AIH. Liver biopsy may be helpful. Small-duct PSC and AMA-negative PBC should be excluded in certain clinical scenarios. Steroids and azathioprine, sometimes with ursodeoxycholic acid, have been used for PSC-AIH. Prognosis may be better than classical PSC, but worse compared to AIH alone. Further studies are warranted to define the optimal approach to diagnosis and management of PSC-AIH. Gastroenterologists and hepatologists should consider overlap with AIH in a patient with PSC and persistently elevated liver enzymes after excluding other etiologies.

Disclosures:
Muaaz Masood, MD1, Asma Siddique, MD1, Rajesh Krishnamoorthi, MD1, Blaire Burman, MD1, Richard Kozarek, MD, FACG2. P2559 - Primary Sclerosing Cholangitis-Autoimmune Hepatitis Overlap Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Virginia Mason Franciscan Health, Seattle, WA; 2Virginia Mason Franciscan Health/Benaroya Research Institute, Seattle, WA
Introduction: Overlap syndromes with autoimmune hepatitis (AIH), primary sclerosing cholangitis (PSC) and primary biliary cirrhosis (PBC) may occur in 3-17% of patients with autoimmune liver disease. PSC-AIH is a rare entity which primarily affects young adults and involves biliary abnormalities of PSC in conjunction with features of AIH.
Case Description/Methods: A 29-year-old male with Crohn’s disease (CD) and biopsy-proven PSC who presented to the Hepatology clinic for persistently elevated liver enzymes. Recent ERCP revealed a mild stricture of the distal common bile duct which was dilated. Brushings were negative for abnormalities by fluorescence in situ hybridization. Repeat MRCP did not reveal biliary abnormalities. The patient reported fatigue, pruritus and dark urine, but denied fevers/chills, abdominal pain, change in bowel habits, weight loss, alcohol use, new medications or supplements. Vital signs were unremarkable. Examination revealed jaundice, scleral icterus and hepatomegaly. Laboratory studies were notable for AST 1091 U/L, ALT 892 U/L, AP 247 U/L, TB 14.1 mg/dL. Due to concern for overlap with AIH, further work-up was obtained which was notable for anti-nuclear antibody >1:640 in a homogeneous nuclear pattern, total IgG 2250 mg/dL, negative antimitochondrial antibody (AMA) and F-actin IgG >100 U. Repeat liver biopsy demonstrated moderate lymphoplasmacytic inflammation, interface activity, lobular necroinflammatory activity, stage II fibrosis – findings suggestive for superimposed AIH. He was started on steroids with resolution of his symptoms and liver enzyme abnormalities. The patient was subsequently switched to azathioprine with an excellent response. Mesalamine for CD was tapered and discontinued.
Discussion: PSC-AIH is considered to be a variant of AIH and is suspected with cholangiographic features of PSC, negative AMA and clinical, biochemical and histological evidence of AIH. No specific diagnostic criteria exist for PSC-AIH. Liver biopsy may be helpful. Small-duct PSC and AMA-negative PBC should be excluded in certain clinical scenarios. Steroids and azathioprine, sometimes with ursodeoxycholic acid, have been used for PSC-AIH. Prognosis may be better than classical PSC, but worse compared to AIH alone. Further studies are warranted to define the optimal approach to diagnosis and management of PSC-AIH. Gastroenterologists and hepatologists should consider overlap with AIH in a patient with PSC and persistently elevated liver enzymes after excluding other etiologies.

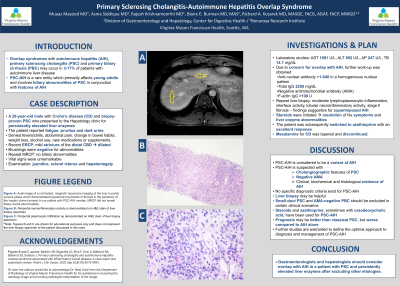
Figure: Axial image of a contrasted, magnetic resonance imaging of the liver in portal venous phase which demonstrated hypoenhancing bands of fibrosis in the periphery of the hepatic dome (arrows) in our patient with PSC-AIH overlap. Magnetic resonance cholangiopancreatography did not reveal biliary ductal abnormalities. Of note, the authors would like to acknowledge Dr. Neal Conti from the Department of Radiology at Virginia Mason Franciscan Health for his assistance in acquiring the radiology image and providing radiologist interpretation of the image.
Disclosures:
Muaaz Masood indicated no relevant financial relationships.
Asma Siddique indicated no relevant financial relationships.
Rajesh Krishnamoorthi indicated no relevant financial relationships.
Blaire Burman indicated no relevant financial relationships.
Richard Kozarek indicated no relevant financial relationships.
Muaaz Masood, MD1, Asma Siddique, MD1, Rajesh Krishnamoorthi, MD1, Blaire Burman, MD1, Richard Kozarek, MD, FACG2. P2559 - Primary Sclerosing Cholangitis-Autoimmune Hepatitis Overlap Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
