Monday Poster Session
Category: Liver
P2563 - Shunt Hunting: Hepatic Encephalopathy in the Absence of Portal Hypertension
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Tricia A. Hengehold, MD
The Ohio State University
Columbus, OH
Presenting Author(s)
Tricia Hengehold, MD1, Megan Mansour, BS2, Chathur Acharya, MBBS3
1The Ohio State University, Columbus, OH; 2The Ohio State University College of Medicine, Columbus, OH; 3Ohio State University, Columbus, OH
Introduction: Recurrent or persistent hepatic encephalopathy (HE) can result from portosystemic shunting, usually seen in the setting of portal hypertension. Congenital vascular malformations or acquired portosystemic bypass shunts can result in Type B HE. These vascular malformations can manifest later in adulthood as recurrent/persistent HE with hyperammonemia, usually in the absence of features of portal hypertension. We discuss 2 cases of non-cirrhotic patients who presented with recurrent Type B HE.
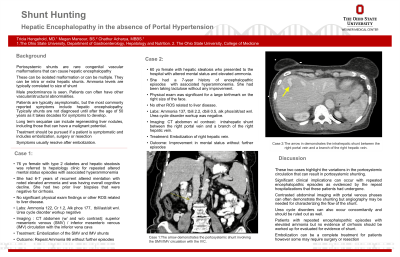
Case Description/Methods: Case 1: 76 yo F with hepatic steatosis presented with multiple episodes of HE with hyperammonemia for the past 6 years. She had 2 prior liver biopsies that were negative for cirrhosis. Workup for urea cycle disorder was negative. CT abdomen (Figure 1, Arrow) with contrast was suggestive of a portosystemic shunt involving the superior mesenteric venous (SMV) / inferior mesenteric venous (IMV) circulation with the inferior vena cava. This was demonstrated on angiography, and she subsequently had embolization of the SMV and IMV portosystemic shunts successfully. Ammonia level decreased post-intervention without further episodes. Case 2: 60 yo F with hepatic steatosis was admitted with a history of recurrent HE and hyperammonemia for the last 7 years, that she had been taking lactulose for with no improvement. Physical exam was significant for a large facial birthmark only. Workup for urea cycle disorder was negative. Her CT abdomen (Figure 2, Arrow) with contrast showed an intrahepatic shunt between the right portal vein and a branch of the right hepatic vein. She had embolization of the right portal vein with sustained improvement in mental status.
Discussion: These cases highlight variations in anatomy of the portosystemic circulation that can result in portosystemic shunting and of the clinical relevance shunts have, due to their presentation as recurrent HE later in adulthood. Recurrent HE with hyperammonemia in adults, in the absence of portal hypertension, should raise the suspicion for the presence of these shunts and prompt contrasted abdominal imaging. Congenital urea cycle abnormalities can present similarly as hyperammonemia in adults and need to be ruled out concomitantly. Contrasted abdominal imaging with portal venous phases can often demonstrate the shunting but angiography may be needed for characterizing the flow of the shunt. Embolization of the shunts are usually without complications and resolve these events, however certain cases may require surgical intervention.

Disclosures:
Tricia Hengehold, MD1, Megan Mansour, BS2, Chathur Acharya, MBBS3. P2563 - Shunt Hunting: Hepatic Encephalopathy in the Absence of Portal Hypertension, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1The Ohio State University, Columbus, OH; 2The Ohio State University College of Medicine, Columbus, OH; 3Ohio State University, Columbus, OH
Introduction: Recurrent or persistent hepatic encephalopathy (HE) can result from portosystemic shunting, usually seen in the setting of portal hypertension. Congenital vascular malformations or acquired portosystemic bypass shunts can result in Type B HE. These vascular malformations can manifest later in adulthood as recurrent/persistent HE with hyperammonemia, usually in the absence of features of portal hypertension. We discuss 2 cases of non-cirrhotic patients who presented with recurrent Type B HE.
Case Description/Methods: Case 1: 76 yo F with hepatic steatosis presented with multiple episodes of HE with hyperammonemia for the past 6 years. She had 2 prior liver biopsies that were negative for cirrhosis. Workup for urea cycle disorder was negative. CT abdomen (Figure 1, Arrow) with contrast was suggestive of a portosystemic shunt involving the superior mesenteric venous (SMV) / inferior mesenteric venous (IMV) circulation with the inferior vena cava. This was demonstrated on angiography, and she subsequently had embolization of the SMV and IMV portosystemic shunts successfully. Ammonia level decreased post-intervention without further episodes. Case 2: 60 yo F with hepatic steatosis was admitted with a history of recurrent HE and hyperammonemia for the last 7 years, that she had been taking lactulose for with no improvement. Physical exam was significant for a large facial birthmark only. Workup for urea cycle disorder was negative. Her CT abdomen (Figure 2, Arrow) with contrast showed an intrahepatic shunt between the right portal vein and a branch of the right hepatic vein. She had embolization of the right portal vein with sustained improvement in mental status.
Discussion: These cases highlight variations in anatomy of the portosystemic circulation that can result in portosystemic shunting and of the clinical relevance shunts have, due to their presentation as recurrent HE later in adulthood. Recurrent HE with hyperammonemia in adults, in the absence of portal hypertension, should raise the suspicion for the presence of these shunts and prompt contrasted abdominal imaging. Congenital urea cycle abnormalities can present similarly as hyperammonemia in adults and need to be ruled out concomitantly. Contrasted abdominal imaging with portal venous phases can often demonstrate the shunting but angiography may be needed for characterizing the flow of the shunt. Embolization of the shunts are usually without complications and resolve these events, however certain cases may require surgical intervention.

Figure: The arrow in Figure A demonstrates the portosystemic shunt involving the SMV/IMV circulation with the IVC. The arrow in Figure B demonstrates the intrahepatic shunt between the right portal vein and a branch of the right hepatic vein.
Disclosures:
Tricia Hengehold indicated no relevant financial relationships.
Megan Mansour indicated no relevant financial relationships.
Chathur Acharya indicated no relevant financial relationships.
Tricia Hengehold, MD1, Megan Mansour, BS2, Chathur Acharya, MBBS3. P2563 - Shunt Hunting: Hepatic Encephalopathy in the Absence of Portal Hypertension, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
