Monday Poster Session
Category: Liver
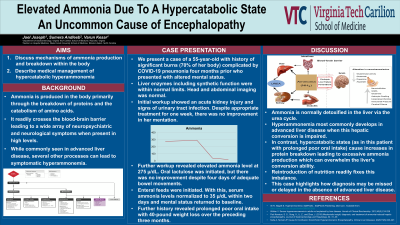
P2565 - Elevated Ammonia Due to Protein Hypercatabolism: An Uncommon Cause of Encephalopathy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- JJ
Joel Joseph, MD
Virginia Tech Carilion School of Medicine
Roanoke, Virginia
Presenting Author(s)
Joel Joseph, MD1, Sumera Andleeb, MBBS, MPH2, Varun Kesar, MD3
1Virginia Tech Carilion School of Medicine, Roanoke, VA; 2Wake Forest University School of Medicine, Winston-Salem, NC; 3Carilion Clinic Virginia Tech, Roanoke, VA
Introduction: Ammonia readily crosses the blood-brain barrier leading to a wide array of neuropsychiatric and neurological symptoms when present in high levels. While commonly seen in advanced liver disease, several other processes can lead to symptomatic hyperammonemia. In one such mechanism, ammonia created by protein catabolism overwhelms the urea cycle leading to elevated serum levels and toxic metabolic encephalopathy.
Case Description/Methods: We present a case of a 55-year-old woman with a history of burns affecting 70% of body area complicated by COVID-19 pneumonia (suffered four months prior to admission) who presented from a nursing facility with altered mental status. Workup on arrival was notable for an acute kidney injury with creatinine elevated at 2.2 mg/dL (from a baseline of 1.0 mg/dL) and signs of urinary tract infection on initial urinalysis. Computerized tomography (CT) of the head did not show any acute intracranial process and CT of the abdomen/pelvis revealed only hepatic steatosis. Her liver enzymes including synthetic function were within normal limits.
She was started on broad-spectrum antibiotics. After one week of appropriate treatment, her mentation failed to improve, and she had continued minimal oral intake. Further workup revealed an elevated ammonia level of 275 µ/dL (normal values 11-51 µ/dL). Lactulose was initiated. Despite four days of adequate bowel movements, there was neither improvement in serum ammonia levels nor her mental status. A nasogastric feeding tube was placed and enteral feeds were initiated. Serum ammonia levels normalized to 35 µ/dL within two days and mental status returned to baseline. Further history revealed prolonged poor oral intake with 40-pound weight loss over the preceding three months. A percutaneous endoscopic gastrostomy tube was placed to continue long-term tube feeds.
Discussion: Ammonia is a byproduct of protein metabolism and is normally detoxified in the liver via the urea cycle, maintaining serum levels below 51 µ/dL. Hyperammonemia most commonly develops in advanced liver disease when this hepatic conversion is impaired. In contrast, hypercatabolic states (as in this patient with prolonged poor oral intake) cause increases in protein breakdown leading to excessive ammonia production which can overwhelm the liver’s conversion ability. Reintroduction of adequate nutrition readily fixes this imbalance. This case highlights how alternative causes of encephalopathy may be missed or delayed in the absence of advanced liver disease.
Disclosures:
Joel Joseph, MD1, Sumera Andleeb, MBBS, MPH2, Varun Kesar, MD3. P2565 - Elevated Ammonia Due to Protein Hypercatabolism: An Uncommon Cause of Encephalopathy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Virginia Tech Carilion School of Medicine, Roanoke, VA; 2Wake Forest University School of Medicine, Winston-Salem, NC; 3Carilion Clinic Virginia Tech, Roanoke, VA
Introduction: Ammonia readily crosses the blood-brain barrier leading to a wide array of neuropsychiatric and neurological symptoms when present in high levels. While commonly seen in advanced liver disease, several other processes can lead to symptomatic hyperammonemia. In one such mechanism, ammonia created by protein catabolism overwhelms the urea cycle leading to elevated serum levels and toxic metabolic encephalopathy.
Case Description/Methods: We present a case of a 55-year-old woman with a history of burns affecting 70% of body area complicated by COVID-19 pneumonia (suffered four months prior to admission) who presented from a nursing facility with altered mental status. Workup on arrival was notable for an acute kidney injury with creatinine elevated at 2.2 mg/dL (from a baseline of 1.0 mg/dL) and signs of urinary tract infection on initial urinalysis. Computerized tomography (CT) of the head did not show any acute intracranial process and CT of the abdomen/pelvis revealed only hepatic steatosis. Her liver enzymes including synthetic function were within normal limits.
She was started on broad-spectrum antibiotics. After one week of appropriate treatment, her mentation failed to improve, and she had continued minimal oral intake. Further workup revealed an elevated ammonia level of 275 µ/dL (normal values 11-51 µ/dL). Lactulose was initiated. Despite four days of adequate bowel movements, there was neither improvement in serum ammonia levels nor her mental status. A nasogastric feeding tube was placed and enteral feeds were initiated. Serum ammonia levels normalized to 35 µ/dL within two days and mental status returned to baseline. Further history revealed prolonged poor oral intake with 40-pound weight loss over the preceding three months. A percutaneous endoscopic gastrostomy tube was placed to continue long-term tube feeds.
Discussion: Ammonia is a byproduct of protein metabolism and is normally detoxified in the liver via the urea cycle, maintaining serum levels below 51 µ/dL. Hyperammonemia most commonly develops in advanced liver disease when this hepatic conversion is impaired. In contrast, hypercatabolic states (as in this patient with prolonged poor oral intake) cause increases in protein breakdown leading to excessive ammonia production which can overwhelm the liver’s conversion ability. Reintroduction of adequate nutrition readily fixes this imbalance. This case highlights how alternative causes of encephalopathy may be missed or delayed in the absence of advanced liver disease.
Disclosures:
Joel Joseph indicated no relevant financial relationships.
Sumera Andleeb indicated no relevant financial relationships.
Varun Kesar indicated no relevant financial relationships.
Joel Joseph, MD1, Sumera Andleeb, MBBS, MPH2, Varun Kesar, MD3. P2565 - Elevated Ammonia Due to Protein Hypercatabolism: An Uncommon Cause of Encephalopathy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
