Monday Poster Session
Category: Liver
P2573 - Tubercular Granulomatous Hepatitis Triggering Hemophagocytic Lymphohistiocytosis: Diagnostic Dilemma and Outcome
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Taif Al-Mansouri, MD
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Taif Al-Mansouri, MD, Mayukh Dey, MD, Calvin Ta, MD, Winn Paing. Soe, MD, Shaurya Sharma, MD, Aruge Lutaf, MD, Stephen Peeke, MD
Maimonides Medical Center, Brooklyn, NY
Introduction: Hemophagocytic Lymphohistiocytosis (HLH) is a rare, hyper-inflammatory condition with a dysregulated immune response. It features an inappropriate activation of the cytotoxic T cells (CTL) and natural killer (NK) cells. The activated NK cells and CTLs lead to excessive cytokine production responsible for multi-organ failure with high mortality. Early diagnosis of HLH poses challenges due to its nonspecific presentation and overlap with diseases serving as a differential of fever of unknown origin. Here we present the case of a 35-year-old Asian male with HLH triggered by tubercular hepatitis.
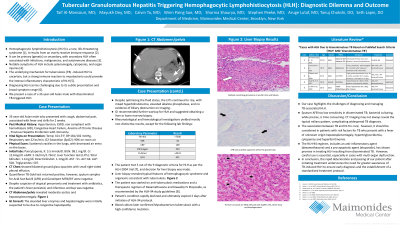
Case Description/Methods: A 35-year-old man with end-stage renal disease, CHF, anemia of chronic disease, and previous hepatitis B infection presented with a 2-week history of fever, cough, and chills. Examination revealed diffuse crackles and decreased air entry on the lung bases. Laboratory tests revealed pancytopenia, transaminitis, high ferritin and triglyceride. Peripheral smear was inconclusive and rheumatological workup unremarkable. Imaging revealed bilateral ground glass opacities with a small right-sided pleural effusion, moderate ascites, and hepatosplenomegaly. Management for pneumonia was initiated. The patient did not show improvement despite efforts to control disease progression. Infectious diseases, rheumatology, pulmonology, gastroenterology, and hematology teams were consulted and consensus was the need for tissue diagnosis. A liver biopsy was obtained demonstrating necrotizing caseating granulomas and erythrophagocytosis, suggestive of tuberculosis with likely HLH pathology.
He was started on anti-tubercular drugs. HLH treatment was initiated using dexamethasone and Etoposide to suppress the hyper-inflammatory immune response and cytokine storm. Despite appropriate treatment, the patient's condition rapidly deteriorated, leading to acute hypoxic respiratory failure secondary to acute respiratory distress syndrome (ARDS) and subsequent demise.
Discussion: This case highlights the challenges in the early diagnosis of HLH. The disease course can be complicated by inflammatory/infectious processes like disseminated TB which then poses a question of immunosuppression in conjunction with anti-TB therapy. This can lead to delays in treatment and a lost opportunity for early disease control. Although there are cases showing benefit of steroids and Etoposide in HLH induced by disseminated TB, further research is needed to determine its efficacy in scenarios complicated by multi-organ dysfunction.
Disclosures:
Taif Al-Mansouri, MD, Mayukh Dey, MD, Calvin Ta, MD, Winn Paing. Soe, MD, Shaurya Sharma, MD, Aruge Lutaf, MD, Stephen Peeke, MD. P2573 - Tubercular Granulomatous Hepatitis Triggering Hemophagocytic Lymphohistiocytosis: Diagnostic Dilemma and Outcome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Maimonides Medical Center, Brooklyn, NY
Introduction: Hemophagocytic Lymphohistiocytosis (HLH) is a rare, hyper-inflammatory condition with a dysregulated immune response. It features an inappropriate activation of the cytotoxic T cells (CTL) and natural killer (NK) cells. The activated NK cells and CTLs lead to excessive cytokine production responsible for multi-organ failure with high mortality. Early diagnosis of HLH poses challenges due to its nonspecific presentation and overlap with diseases serving as a differential of fever of unknown origin. Here we present the case of a 35-year-old Asian male with HLH triggered by tubercular hepatitis.
Case Description/Methods: A 35-year-old man with end-stage renal disease, CHF, anemia of chronic disease, and previous hepatitis B infection presented with a 2-week history of fever, cough, and chills. Examination revealed diffuse crackles and decreased air entry on the lung bases. Laboratory tests revealed pancytopenia, transaminitis, high ferritin and triglyceride. Peripheral smear was inconclusive and rheumatological workup unremarkable. Imaging revealed bilateral ground glass opacities with a small right-sided pleural effusion, moderate ascites, and hepatosplenomegaly. Management for pneumonia was initiated. The patient did not show improvement despite efforts to control disease progression. Infectious diseases, rheumatology, pulmonology, gastroenterology, and hematology teams were consulted and consensus was the need for tissue diagnosis. A liver biopsy was obtained demonstrating necrotizing caseating granulomas and erythrophagocytosis, suggestive of tuberculosis with likely HLH pathology.
He was started on anti-tubercular drugs. HLH treatment was initiated using dexamethasone and Etoposide to suppress the hyper-inflammatory immune response and cytokine storm. Despite appropriate treatment, the patient's condition rapidly deteriorated, leading to acute hypoxic respiratory failure secondary to acute respiratory distress syndrome (ARDS) and subsequent demise.
Discussion: This case highlights the challenges in the early diagnosis of HLH. The disease course can be complicated by inflammatory/infectious processes like disseminated TB which then poses a question of immunosuppression in conjunction with anti-TB therapy. This can lead to delays in treatment and a lost opportunity for early disease control. Although there are cases showing benefit of steroids and Etoposide in HLH induced by disseminated TB, further research is needed to determine its efficacy in scenarios complicated by multi-organ dysfunction.
Disclosures:
Taif Al-Mansouri indicated no relevant financial relationships.
Mayukh Dey indicated no relevant financial relationships.
Calvin Ta indicated no relevant financial relationships.
Winn Soe indicated no relevant financial relationships.
Shaurya Sharma indicated no relevant financial relationships.
Aruge Lutaf indicated no relevant financial relationships.
Stephen Peeke indicated no relevant financial relationships.
Taif Al-Mansouri, MD, Mayukh Dey, MD, Calvin Ta, MD, Winn Paing. Soe, MD, Shaurya Sharma, MD, Aruge Lutaf, MD, Stephen Peeke, MD. P2573 - Tubercular Granulomatous Hepatitis Triggering Hemophagocytic Lymphohistiocytosis: Diagnostic Dilemma and Outcome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
