Monday Poster Session
Category: Liver
P2583 - Hepatic Primary Amyloidosis: A Rare Cause of Cholestatic Liver Injury
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sumedha Singh, MD
Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Sumedha Singh, MD, Richard Kalman, MD
Einstein Medical Center, Philadelphia, PA
Introduction: Cholestatic liver injury is recognized by elevation in ALP and bilirubin on serology. It often occurs due to obstruction or inflammation of the biliary tracts. When this pattern occurs, the differential includes: biliary obstruction, infection, drug-induced liver injury, autoimmune disease, infiltrative disease, and malignancy. We present a patient who presented with abnormal liver chemistries and jaundice and found to have primary systemic amyloidosis with hepatic involvement. We highlight consideration of rare infiltrative diseases such as amyloidosis in patients presenting with cholestasis and hepatomegaly.
Case Description/Methods: 65M with hypertension, former smoker presented for evaluation of abnormal liver chemistries. He was noted to have jaundice, pruritus, dark urine, and significant weight loss. His bloodwork was remarkable for AST 241, ALT 140, ALP 1,221, TBili 22.9 (Direct 14.5), Cr 2.34. Bloodwork was negative for chronic hepatitis B or C, autoimmune liver disease, hemochromatosis. Urine showed dark urine with high bilirubin and high protein. CT imaging was remarkable for two lung masses of 2 cm and 1 cm and inhomogeneous attenuation of the liver. MRI showed no evidence of biliary obstruction or inflammation and heterogeneous enhancement of hepatic parenchyma without cirrhosis or focal liver mass. PET scan suggested no active malignancy. Liver biopsy was performed. Patient also had dysphagia and underwent EGD. Biopsies of the stomach and esophagus resulted with positive Congo red stains indicating a diagnosis of amyloidosis. The liver and abdominal fat pad biopsies were also consistent with amyloidosis. Oncology was engaged and patient was recommended to start chemotherapy with daratumumab, bortezoib, cyclophosphamide, and dexamethasone, pending a bone marrow biopsy. However, due to the patient’s performance status and contraindication to therapy from renal and liver failure, bone marrow biopsy was not pursued. The patient was discharged on home hospice days later.
Discussion: Primary (AL) amyloidosis is a rare infiltrative systemic disease. Amyloidosis is an important differential to consider when there is systemic organ injury with cholestatic hepatic injury. In addition to hepatomegaly and weight loss, elevated ALP and proteinuria may be additional clues in diagnosis. Frequently, the diagnosis of AL is obtained when disease is extensive with poor life expectancy. The option for systemic chemotherapy may be available to some patients but therapeutic benefit is unclear.

Disclosures:
Sumedha Singh, MD, Richard Kalman, MD. P2583 - Hepatic Primary Amyloidosis: A Rare Cause of Cholestatic Liver Injury, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Einstein Medical Center, Philadelphia, PA
Introduction: Cholestatic liver injury is recognized by elevation in ALP and bilirubin on serology. It often occurs due to obstruction or inflammation of the biliary tracts. When this pattern occurs, the differential includes: biliary obstruction, infection, drug-induced liver injury, autoimmune disease, infiltrative disease, and malignancy. We present a patient who presented with abnormal liver chemistries and jaundice and found to have primary systemic amyloidosis with hepatic involvement. We highlight consideration of rare infiltrative diseases such as amyloidosis in patients presenting with cholestasis and hepatomegaly.
Case Description/Methods: 65M with hypertension, former smoker presented for evaluation of abnormal liver chemistries. He was noted to have jaundice, pruritus, dark urine, and significant weight loss. His bloodwork was remarkable for AST 241, ALT 140, ALP 1,221, TBili 22.9 (Direct 14.5), Cr 2.34. Bloodwork was negative for chronic hepatitis B or C, autoimmune liver disease, hemochromatosis. Urine showed dark urine with high bilirubin and high protein. CT imaging was remarkable for two lung masses of 2 cm and 1 cm and inhomogeneous attenuation of the liver. MRI showed no evidence of biliary obstruction or inflammation and heterogeneous enhancement of hepatic parenchyma without cirrhosis or focal liver mass. PET scan suggested no active malignancy. Liver biopsy was performed. Patient also had dysphagia and underwent EGD. Biopsies of the stomach and esophagus resulted with positive Congo red stains indicating a diagnosis of amyloidosis. The liver and abdominal fat pad biopsies were also consistent with amyloidosis. Oncology was engaged and patient was recommended to start chemotherapy with daratumumab, bortezoib, cyclophosphamide, and dexamethasone, pending a bone marrow biopsy. However, due to the patient’s performance status and contraindication to therapy from renal and liver failure, bone marrow biopsy was not pursued. The patient was discharged on home hospice days later.
Discussion: Primary (AL) amyloidosis is a rare infiltrative systemic disease. Amyloidosis is an important differential to consider when there is systemic organ injury with cholestatic hepatic injury. In addition to hepatomegaly and weight loss, elevated ALP and proteinuria may be additional clues in diagnosis. Frequently, the diagnosis of AL is obtained when disease is extensive with poor life expectancy. The option for systemic chemotherapy may be available to some patients but therapeutic benefit is unclear.

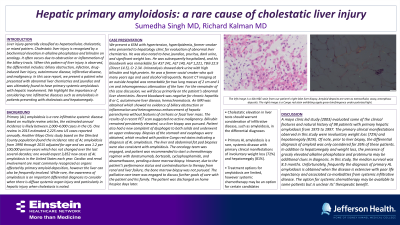
Figure: The image below is a 40x H&E stain from our patient’s right-lobe liver biopsy. Amyloid deposits are seen as extracellular, waxy, amorphous deposits
Disclosures:
Sumedha Singh indicated no relevant financial relationships.
Richard Kalman indicated no relevant financial relationships.
Sumedha Singh, MD, Richard Kalman, MD. P2583 - Hepatic Primary Amyloidosis: A Rare Cause of Cholestatic Liver Injury, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
