Monday Poster Session
Category: Liver
P2602 - Hepatic Encephalopathy Secondary to Non-Cirrhotic Portosystemic Shunt
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- BT
Bhavi Trivedi, MD
Texas Tech University Health Sciences Center
El Paso, Texas
Presenting Author(s)
Bhavi Trivedi, MD1, Amish Parikh, DO2, Monica Botros, MD1, Brian Lee, DO1, Jeff Angelo Taclob, MD1, Shaked Laks, MD3, Alejandro Robles, MD3, Marc Zuckerman, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Huntington Hospital, Pasadena, CA; 3Texas Tech, El Paso, TX
Introduction: Hepatic encephalopathy is a common complication seen in patients with cirrhosis, although a very uncommon pathology in the absence of cirrhosis. Non-cirrhotic portosystemic shunt formation is a rare condition that may go undetected due to its resemblance to hyperammonemia-induced hepatic encephalopathy. These patients often have normal liver function tests and lack the common signs of cirrhosis. Therefore, they are frequently misdiagnosed with psychiatric disorders or dementia, resulting in suboptimal treatment and a negative impact on their quality of life.
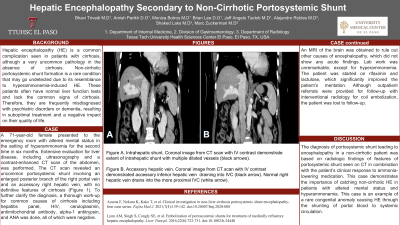
Case Description/Methods: A 71-year-old female presented to the emergency room with altered mental status in the setting of hyperammonemia for the second time in six months. Extensive evaluation for liver disease, including ultrasonography and a contrast-enhanced CT scan of the abdomen, was performed. The CT scan revealed an uncommon portosystemic shunt involving an enlarged posterior branch of the right portal vein and an accessory right hepatic vein, with no definitive features of cirrhosis (Figure 1). To further clarify the diagnosis, a thorough work-up for common causes of cirrhosis including hepatitis panel, HIV levels, ceruloplasmin, antimitochondrial antibody, alpha-1 antitrypsin, ANA, and hepatitis panel was done, all of which were negative. An MRI of the brain was obtained to rule out other causes of encephalopathy, which did not show any acute findings. Lab work was unremarkable, except for hyperammonemia. The patient was started on ammonia-lowering therapy, which significantly improved the patient’s mentation. Although outpatient referrals were provided for follow-up with interventional radiology for coil embolization, the patient was lost to follow-up.
Discussion: The diagnosis of portosystemic shunt leading to encephalopathy in a non-cirrhotic patient was based on radiologic findings of features of portosystemic shunt seen on CT in combination with the patient’s clinical response to ammonia-lowering medication. This case demonstrates the importance of catching non-cirrhotic hepatic encephalopathy in patients with altered mental status and hyperammonemia. This case is an example of a rare congenital anomaly causing HE through the shunting of portal blood to systemic circulation.

Disclosures:
Bhavi Trivedi, MD1, Amish Parikh, DO2, Monica Botros, MD1, Brian Lee, DO1, Jeff Angelo Taclob, MD1, Shaked Laks, MD3, Alejandro Robles, MD3, Marc Zuckerman, MD1. P2602 - Hepatic Encephalopathy Secondary to Non-Cirrhotic Portosystemic Shunt, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, TX; 2Huntington Hospital, Pasadena, CA; 3Texas Tech, El Paso, TX
Introduction: Hepatic encephalopathy is a common complication seen in patients with cirrhosis, although a very uncommon pathology in the absence of cirrhosis. Non-cirrhotic portosystemic shunt formation is a rare condition that may go undetected due to its resemblance to hyperammonemia-induced hepatic encephalopathy. These patients often have normal liver function tests and lack the common signs of cirrhosis. Therefore, they are frequently misdiagnosed with psychiatric disorders or dementia, resulting in suboptimal treatment and a negative impact on their quality of life.
Case Description/Methods: A 71-year-old female presented to the emergency room with altered mental status in the setting of hyperammonemia for the second time in six months. Extensive evaluation for liver disease, including ultrasonography and a contrast-enhanced CT scan of the abdomen, was performed. The CT scan revealed an uncommon portosystemic shunt involving an enlarged posterior branch of the right portal vein and an accessory right hepatic vein, with no definitive features of cirrhosis (Figure 1). To further clarify the diagnosis, a thorough work-up for common causes of cirrhosis including hepatitis panel, HIV levels, ceruloplasmin, antimitochondrial antibody, alpha-1 antitrypsin, ANA, and hepatitis panel was done, all of which were negative. An MRI of the brain was obtained to rule out other causes of encephalopathy, which did not show any acute findings. Lab work was unremarkable, except for hyperammonemia. The patient was started on ammonia-lowering therapy, which significantly improved the patient’s mentation. Although outpatient referrals were provided for follow-up with interventional radiology for coil embolization, the patient was lost to follow-up.
Discussion: The diagnosis of portosystemic shunt leading to encephalopathy in a non-cirrhotic patient was based on radiologic findings of features of portosystemic shunt seen on CT in combination with the patient’s clinical response to ammonia-lowering medication. This case demonstrates the importance of catching non-cirrhotic hepatic encephalopathy in patients with altered mental status and hyperammonemia. This case is an example of a rare congenital anomaly causing HE through the shunting of portal blood to systemic circulation.

Figure: Contiguous axial images of a CT scan of the abdomen and pelvis with IV contrast (A,B,C). There is a communication of the right portal vein (black arrow) with an accessory inferior hepatic vein (white arrow) via a dilated intrahepatic vessel (black arrowhead).
Disclosures:
Bhavi Trivedi indicated no relevant financial relationships.
Amish Parikh indicated no relevant financial relationships.
Monica Botros indicated no relevant financial relationships.
Brian Lee indicated no relevant financial relationships.
Jeff Angelo Taclob indicated no relevant financial relationships.
Shaked Laks indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Marc Zuckerman indicated no relevant financial relationships.
Bhavi Trivedi, MD1, Amish Parikh, DO2, Monica Botros, MD1, Brian Lee, DO1, Jeff Angelo Taclob, MD1, Shaked Laks, MD3, Alejandro Robles, MD3, Marc Zuckerman, MD1. P2602 - Hepatic Encephalopathy Secondary to Non-Cirrhotic Portosystemic Shunt, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
