Monday Poster Session
Category: Small Intestine
P2655 - A Rare Case of Sepsis Due to Entamoeba histolytica Amebiasis With Concurrent Intra and Extra-Intestinal Manifestations
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Hamza Chaudhry, MD
Weill Cornell Medical College
Friendswood, TX
Presenting Author(s)
Hamza Chaudhry, MD1, Mohammad I. Bhatti, 2, Lasha Gogokhia, MD3, Benjamin Gordon, MD4, David Wan, BS, MD5
1Weill Cornell Medical College, Friendswood, TX; 2Weill Cornell Medicine-Qatar, Doha, Ad Dawhah, Qatar; 3New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 4New York Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 5Weill Cornell Medicine, New York, NY
Introduction: Entamoeba histolytica is a protozoan transmitted through the fecal-oral route that causes asymptomatic infection in 90% of cases but can lead to amebic dysentery and extra-intestinal manifestations. Here, we report a case of a patient who presented with fevers and abdominal pain found to have sepsis and amebic dysentery with multiple liver abscesses due to E. histolytica further complicated by an upper gastrointestinal (GI) bleed.
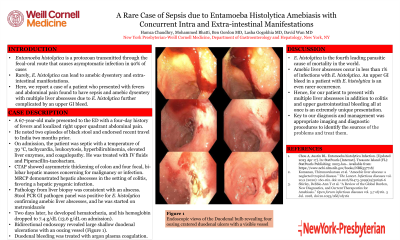
Case Description/Methods: A 67-year-old male with hypertension and hyperlipidemia presented to the ED with a four-day history of fevers and localized right upper quadrant abdominal pain. He noted two episodes of black stool and endorsed recent travel to India two months prior. On admission, the patient was septic with a temperature of 39 °C, tachycardia, leukocytosis, hyperbilirubinemia, elevated liver enzymes, and coagulopathy. He was treated with IV fluids and broad-spectrum antibacterial therapy (Piperacillin-tazobactam). Abdominal Computer Topography showed asymmetric thickening of colon and four focal, bi-lobar hepatic masses concerning for malignancy or infection. Subsequent Magnetic resonance cholangiopancreatography (MRCP) demonstrated hepatic abscesses in the setting of colitis, favoring a hepatic pyogenic infection. Pathology from liver biopsy was consistent with an abscess. The following day, stool PCR gastrointestinal pathogen panel was positive for E. histolytica confirming amebic liver abscesses, and he was started on metronidazole. However, two days later, he developed hematochezia, and his hemoglobin dropped to 7.4 g/dL (13.6 g/dL on admission). Bidirectional endoscopy revealed large shallow duodenal ulcerations with an oozing vessel (Figure 1). The duodenal bleeding was treated with argon plasma coagulation. The patient improved clinically and was deemed stable for discharge.
Discussion: E. histolytica is the fourth leading parasitic cause of mortality in the world. Amebic liver abscesses occur in less than 1% of infections with E. histolytica. An upper GI bleed in a patient with E. histolytica is an even rarer occurrence. Hence, for our patient to present with multiple liver abscesses in addition to colitis and upper gastrointestinal bleeding all at once is an extremely unique presentation. Key to our diagnosis and management was appropriate imaging and diagnostic procedures to identify the sources of the problems and treat them.

Disclosures:
Hamza Chaudhry, MD1, Mohammad I. Bhatti, 2, Lasha Gogokhia, MD3, Benjamin Gordon, MD4, David Wan, BS, MD5. P2655 - A Rare Case of Sepsis Due to Entamoeba histolytica Amebiasis With Concurrent Intra and Extra-Intestinal Manifestations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Weill Cornell Medical College, Friendswood, TX; 2Weill Cornell Medicine-Qatar, Doha, Ad Dawhah, Qatar; 3New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 4New York Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 5Weill Cornell Medicine, New York, NY
Introduction: Entamoeba histolytica is a protozoan transmitted through the fecal-oral route that causes asymptomatic infection in 90% of cases but can lead to amebic dysentery and extra-intestinal manifestations. Here, we report a case of a patient who presented with fevers and abdominal pain found to have sepsis and amebic dysentery with multiple liver abscesses due to E. histolytica further complicated by an upper gastrointestinal (GI) bleed.
Case Description/Methods: A 67-year-old male with hypertension and hyperlipidemia presented to the ED with a four-day history of fevers and localized right upper quadrant abdominal pain. He noted two episodes of black stool and endorsed recent travel to India two months prior. On admission, the patient was septic with a temperature of 39 °C, tachycardia, leukocytosis, hyperbilirubinemia, elevated liver enzymes, and coagulopathy. He was treated with IV fluids and broad-spectrum antibacterial therapy (Piperacillin-tazobactam). Abdominal Computer Topography showed asymmetric thickening of colon and four focal, bi-lobar hepatic masses concerning for malignancy or infection. Subsequent Magnetic resonance cholangiopancreatography (MRCP) demonstrated hepatic abscesses in the setting of colitis, favoring a hepatic pyogenic infection. Pathology from liver biopsy was consistent with an abscess. The following day, stool PCR gastrointestinal pathogen panel was positive for E. histolytica confirming amebic liver abscesses, and he was started on metronidazole. However, two days later, he developed hematochezia, and his hemoglobin dropped to 7.4 g/dL (13.6 g/dL on admission). Bidirectional endoscopy revealed large shallow duodenal ulcerations with an oozing vessel (Figure 1). The duodenal bleeding was treated with argon plasma coagulation. The patient improved clinically and was deemed stable for discharge.
Discussion: E. histolytica is the fourth leading parasitic cause of mortality in the world. Amebic liver abscesses occur in less than 1% of infections with E. histolytica. An upper GI bleed in a patient with E. histolytica is an even rarer occurrence. Hence, for our patient to present with multiple liver abscesses in addition to colitis and upper gastrointestinal bleeding all at once is an extremely unique presentation. Key to our diagnosis and management was appropriate imaging and diagnostic procedures to identify the sources of the problems and treat them.

Figure: Figure 1. Endoscopic views of the Duodenal bulb revealing four oozing cratered duodenal ulcers with a visible vessel
Disclosures:
Hamza Chaudhry indicated no relevant financial relationships.
Mohammad Bhatti indicated no relevant financial relationships.
Lasha Gogokhia indicated no relevant financial relationships.
Benjamin Gordon indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Hamza Chaudhry, MD1, Mohammad I. Bhatti, 2, Lasha Gogokhia, MD3, Benjamin Gordon, MD4, David Wan, BS, MD5. P2655 - A Rare Case of Sepsis Due to Entamoeba histolytica Amebiasis With Concurrent Intra and Extra-Intestinal Manifestations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
