Monday Poster Session
Category: Small Intestine
P2664 - Not Your Usual Duodenal Pearls: Unveiling the True Nature of a Supposed Duodenal Type Follicular Lymphoma as a Classic Follicular Lymphoma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Mahak Chauhan, MD
University of Arizona-Tucson College of Medicine
Tucson, AZ
Presenting Author(s)
Award: Presidential Poster Award
Brandon Witten, MD1, Mahak Chauhan, MD1, Alex Heimbigner, MD2, Avin Aggarwal, MBBS3
1University of Arizona-Tucson College of Medicine, Tucson, AZ; 2Banner University Medical Center, Tucson, AZ; 3University of Arizona College of Medicine, Tucson, AZ
Introduction: Duodenal type follicular lymphoma (DTFL) might resemble lymphangiectasias on esophagogastroduodenoscopy (EGD). With growing rates of EGDs, DTFL detection has increased. It is now recognized as a distinct entity from classic-follicular lymphoma (cFL) of the gastrointestinal (GI) tract. Typically DTFL is asymptomatic, incidentally found on EGDs and histopathological graded as 1-21. We describe a case of cFL (grade 3A) confined to the duodenum initially diagnosed as DTFL.
Case Description/Methods: A 34-year-old female with a history of H. pylori-related duodenal ulcers presented with epigastric pain associated with 20 lbs weight loss, intermittent nausea and vomiting for 2 months. 5 years prior EGD showed moderate chronic nonspecific duodenitis.
EGD was performed for nonspecific dyspepsia. Results were unremarkable aside from white nodular grouped polypoidal lesions in the duodenum initially appearing as lymphangiectasias. Biopsies noted atypical nodular infiltrate of small cleaved lymphoid cells that aberrantly expressed BCL-2, low Ki-67 proliferation index, and margination of the follicular dendritic cells by CD21. Histopathology was consistent with DTFL. Given initial biopsies, push enteroscopy and colonoscopy were performed. Enteroscopy showed punctate white lesions throughout the duodenum prompting repeat biopsies; colonoscopy was unremarkable.
Repeat pathology findings revealed over 15 centroblasts per high power field intermixed with centrocytes, consistent with grade 3A cFL. This change reflected disease progression or sampling bias; the final diagnosis was revised. Bone marrow analysis, flow cytometry and PET scan were negative for diffuse lymphoma. Treatment with rituximab was started.
Discussion: Differential diagnosis for white nodular lesions in the duodenum on EGD include lymphangiectasia, DTFL or cFL. All three diagnoses, while endoscopically similar differ greatly. While DTFL is usually indolent, cFL confined to the GI tract can display transmural infiltration and systemic spread1. Hence, the multidisciplinary involvement of hematopathologists, oncologists, and radiologists is critical for an accurate diagnosis.
References:
1) Kurz, Katrin S et al. “Follicular Lymphoma in the 5th Edition of the WHO-Classification of Haematolymphoid Neoplasms-Updated Classification and New Biological Data.” Cancers vol. 15,3 785. 27 Jan. 2023.

Disclosures:
Brandon Witten, MD1, Mahak Chauhan, MD1, Alex Heimbigner, MD2, Avin Aggarwal, MBBS3. P2664 - Not Your Usual Duodenal Pearls: Unveiling the True Nature of a Supposed Duodenal Type Follicular Lymphoma as a Classic Follicular Lymphoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Brandon Witten, MD1, Mahak Chauhan, MD1, Alex Heimbigner, MD2, Avin Aggarwal, MBBS3
1University of Arizona-Tucson College of Medicine, Tucson, AZ; 2Banner University Medical Center, Tucson, AZ; 3University of Arizona College of Medicine, Tucson, AZ
Introduction: Duodenal type follicular lymphoma (DTFL) might resemble lymphangiectasias on esophagogastroduodenoscopy (EGD). With growing rates of EGDs, DTFL detection has increased. It is now recognized as a distinct entity from classic-follicular lymphoma (cFL) of the gastrointestinal (GI) tract. Typically DTFL is asymptomatic, incidentally found on EGDs and histopathological graded as 1-21. We describe a case of cFL (grade 3A) confined to the duodenum initially diagnosed as DTFL.
Case Description/Methods: A 34-year-old female with a history of H. pylori-related duodenal ulcers presented with epigastric pain associated with 20 lbs weight loss, intermittent nausea and vomiting for 2 months. 5 years prior EGD showed moderate chronic nonspecific duodenitis.
EGD was performed for nonspecific dyspepsia. Results were unremarkable aside from white nodular grouped polypoidal lesions in the duodenum initially appearing as lymphangiectasias. Biopsies noted atypical nodular infiltrate of small cleaved lymphoid cells that aberrantly expressed BCL-2, low Ki-67 proliferation index, and margination of the follicular dendritic cells by CD21. Histopathology was consistent with DTFL. Given initial biopsies, push enteroscopy and colonoscopy were performed. Enteroscopy showed punctate white lesions throughout the duodenum prompting repeat biopsies; colonoscopy was unremarkable.
Repeat pathology findings revealed over 15 centroblasts per high power field intermixed with centrocytes, consistent with grade 3A cFL. This change reflected disease progression or sampling bias; the final diagnosis was revised. Bone marrow analysis, flow cytometry and PET scan were negative for diffuse lymphoma. Treatment with rituximab was started.
Discussion: Differential diagnosis for white nodular lesions in the duodenum on EGD include lymphangiectasia, DTFL or cFL. All three diagnoses, while endoscopically similar differ greatly. While DTFL is usually indolent, cFL confined to the GI tract can display transmural infiltration and systemic spread1. Hence, the multidisciplinary involvement of hematopathologists, oncologists, and radiologists is critical for an accurate diagnosis.
References:
1) Kurz, Katrin S et al. “Follicular Lymphoma in the 5th Edition of the WHO-Classification of Haematolymphoid Neoplasms-Updated Classification and New Biological Data.” Cancers vol. 15,3 785. 27 Jan. 2023.

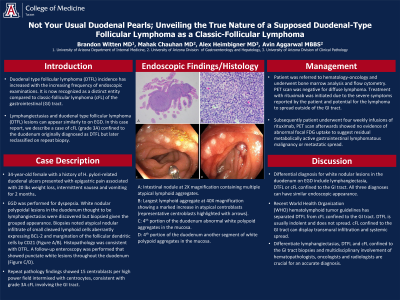
Figure: A: Intestinal nodule at 2x, containing multiple atypical lymphoid aggregates.
B: Largest lymphoid aggregate at 40x, showing a marked increase in atypical centroblasts (representative centroblasts highlighted with arrows)
C: 4th portion of the duodenum abnormal white polypoid aggregates in the mucosa.
D: 4th portion of the duodenum another segment of white polypoid aggregates in the mucosa.
B: Largest lymphoid aggregate at 40x, showing a marked increase in atypical centroblasts (representative centroblasts highlighted with arrows)
C: 4th portion of the duodenum abnormal white polypoid aggregates in the mucosa.
D: 4th portion of the duodenum another segment of white polypoid aggregates in the mucosa.
Disclosures:
Brandon Witten indicated no relevant financial relationships.
Mahak Chauhan indicated no relevant financial relationships.
Alex Heimbigner indicated no relevant financial relationships.
Avin Aggarwal indicated no relevant financial relationships.
Brandon Witten, MD1, Mahak Chauhan, MD1, Alex Heimbigner, MD2, Avin Aggarwal, MBBS3. P2664 - Not Your Usual Duodenal Pearls: Unveiling the True Nature of a Supposed Duodenal Type Follicular Lymphoma as a Classic Follicular Lymphoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

