Monday Poster Session
Category: Small Intestine
P2682 - Bleeding GIST Suggestive of Undiagnosed Neurofibromatosis Type 1
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- JZ
Justin Zhuo, MD
Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Justin Zhuo, MD1, Ping He, MD, PhD1, Mahmoud Ali, MBBCh1, Anish V. Patel, MD1, Keerthana Kesavarapu, DO2
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Robert Wood Johnson University Hospital, New Brunswick, NJ
Introduction: Neurofibromatosis type 1 (NF1) is one of the most common autosomal dominant genetic disorders. Patients with NF1 have a higher risk of developing gastrointestinal stromal tumors (GISTs). We describe a case of a jejunal GIST discovered during endoscopic evaluation for severe gastrointestinal (GI) bleeding in a young adult.
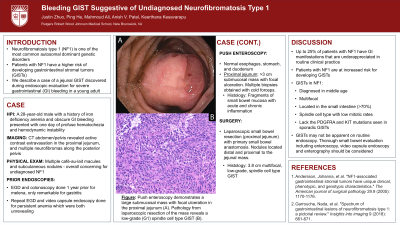
Case Description/Methods: A 28-year-old male with a history of iron deficiency anemia and obscure GI bleeding presented with one day of profuse hematochezia and hemodynamic instability. CT revealed active contrast extravasation in the proximal jejunum and multiple neurofibromas along the posterior pelvis. Physical exam revealed multiple café-au-lait macules and subcutaneous nodules, which were overall concerning for undiagnosed NF1. Prior endoscopic evaluation included EGD and colonoscopy performed one year ago for melena, which revealed gastritis. Due to ongoing anemia, repeat EGD and video capsule endoscopy had also been performed and were nondiagnostic. Therefore, we performed a push enteroscopy which demonstrated a large submucosal mass with focal ulceration in the proximal jejunum (1A). Cold forceps biopsies revealed fragments of small bowel mucosa with acute and chronic inflammation. The patient underwent laparoscopic resection of a segment of proximal jejunum containing the 3.8 cm mass with nodules distal and proximal to it. Pathology was consistent with a low-risk, multifocal, spindle cell type GIST (1B). Without further GI bleeding, the patient was discharged and referred for genetic counseling.
Discussion: While NF1 is most commonly recognized by café-au-lait macules and cutaneous neurofibromas, up to 25% of patients have GI manifestations that are often underappreciated in routine clinical practice. GISTs associated with NF1 are often diagnosed in middle age, multifocal, located in the small intestine ( >70%), have spindle cells with low mitotic rates, and lack the PDGFRA and KIT mutations typically seen in sporadic GIST. Patients with wild-type GIST occurring at a younger age should be examined for neurocutaneous markers and a complete family history. Our patient had been experiencing significant GI bleeding and anemia for over a year prior to his diagnosis, highlighting the underrecognition of NF1 features and the importance of GI findings in identifying patients with undiagnosed NF1. GISTs in NF1 may not be apparent on routine endoscopy. Thorough small bowel evaluation including enteroscopy, video capsule endoscopy and enterography should be considered.

Disclosures:
Justin Zhuo, MD1, Ping He, MD, PhD1, Mahmoud Ali, MBBCh1, Anish V. Patel, MD1, Keerthana Kesavarapu, DO2. P2682 - Bleeding GIST Suggestive of Undiagnosed Neurofibromatosis Type 1, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Robert Wood Johnson University Hospital, New Brunswick, NJ
Introduction: Neurofibromatosis type 1 (NF1) is one of the most common autosomal dominant genetic disorders. Patients with NF1 have a higher risk of developing gastrointestinal stromal tumors (GISTs). We describe a case of a jejunal GIST discovered during endoscopic evaluation for severe gastrointestinal (GI) bleeding in a young adult.
Case Description/Methods: A 28-year-old male with a history of iron deficiency anemia and obscure GI bleeding presented with one day of profuse hematochezia and hemodynamic instability. CT revealed active contrast extravasation in the proximal jejunum and multiple neurofibromas along the posterior pelvis. Physical exam revealed multiple café-au-lait macules and subcutaneous nodules, which were overall concerning for undiagnosed NF1. Prior endoscopic evaluation included EGD and colonoscopy performed one year ago for melena, which revealed gastritis. Due to ongoing anemia, repeat EGD and video capsule endoscopy had also been performed and were nondiagnostic. Therefore, we performed a push enteroscopy which demonstrated a large submucosal mass with focal ulceration in the proximal jejunum (1A). Cold forceps biopsies revealed fragments of small bowel mucosa with acute and chronic inflammation. The patient underwent laparoscopic resection of a segment of proximal jejunum containing the 3.8 cm mass with nodules distal and proximal to it. Pathology was consistent with a low-risk, multifocal, spindle cell type GIST (1B). Without further GI bleeding, the patient was discharged and referred for genetic counseling.
Discussion: While NF1 is most commonly recognized by café-au-lait macules and cutaneous neurofibromas, up to 25% of patients have GI manifestations that are often underappreciated in routine clinical practice. GISTs associated with NF1 are often diagnosed in middle age, multifocal, located in the small intestine ( >70%), have spindle cells with low mitotic rates, and lack the PDGFRA and KIT mutations typically seen in sporadic GIST. Patients with wild-type GIST occurring at a younger age should be examined for neurocutaneous markers and a complete family history. Our patient had been experiencing significant GI bleeding and anemia for over a year prior to his diagnosis, highlighting the underrecognition of NF1 features and the importance of GI findings in identifying patients with undiagnosed NF1. GISTs in NF1 may not be apparent on routine endoscopy. Thorough small bowel evaluation including enteroscopy, video capsule endoscopy and enterography should be considered.

Figure: Push enteroscopy demonstrates a large GIST in the proximal jejunum (A). Histology reveals spindle cells with a low mitotic rate (B)
Disclosures:
Justin Zhuo indicated no relevant financial relationships.
Ping He indicated no relevant financial relationships.
Mahmoud Ali indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Keerthana Kesavarapu indicated no relevant financial relationships.
Justin Zhuo, MD1, Ping He, MD, PhD1, Mahmoud Ali, MBBCh1, Anish V. Patel, MD1, Keerthana Kesavarapu, DO2. P2682 - Bleeding GIST Suggestive of Undiagnosed Neurofibromatosis Type 1, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
