Monday Poster Session
Category: Small Intestine
P2699 - Whipple's Disease with Dermatologic Manifestations
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- VJ
Vivek V. Jasti, MD
OhioHealth Riverside Methodist Hospital
Columbus, OH
Presenting Author(s)
Vivek V. Jasti, MD1, Jessica Barrett, DO2, Marty M. Meyer, MD3, Jessica A.. Hemminger, MD4, Shail Govani, MD, MSc5
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2OhioHealth, Columbus, OH; 3Ohio Gastroenterology Group, Inc., Dublin, OH; 4Mount Carmel Health System, Columbus, OH; 5Ohio Gastroenterology Group, Inc., Columbus, OH
Introduction: Whipple’s disease (WD) is a rare, chronic infection due to Tropheryma whipplei (TW). Symptoms are non-specific and progress slowly. We present a case of WD with abnormal skin findings.
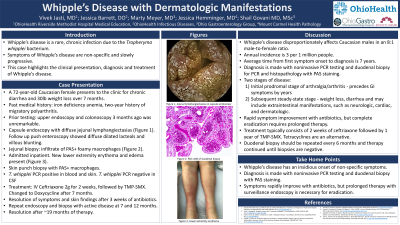
Case Description/Methods: A 72-year-old Caucasian female with a 2-year history of migratory polyarthritis presented for workup of chronic diarrhea, iron deficiency anemia, and 30lb weight loss over 7 months. Recent upper endoscopy and colonoscopy for anemia was unremarkable. Capsule endoscopy revealed jejunal lymphangiectasias. Follow up push enteroscopy showed diffuse dilated lacteals and villous blunting. Duodenal and jejunal mucosal biopsies contained an extensive infiltrate of PAS-positive foamy macrophages in the lamina propria. TW PCR was positive, confirming WD. Inpatient admission was arranged, at which time new lower extremity erythema and edema was noted. Punch biopsy of the skin lesion also revealed PAS-positive macrophages. Skin and blood were TW PCR positive. Lumbar puncture was performed; CSF PCR was negative. Treatment was started with IV ceftriaxone 2g daily for 2 weeks followed by trimethoprim-sulfamethoxazole (TMP-SMX). After 3 weeks the patient reported symptomatic and dermatologic improvement. Due to asymptomatic alkaline phosphatase elevation, TMP-SMX was changed to doxycycline after 7 months. Repeat endoscopy and biopsy at 7 and 12 months revealed active disease. After 9 more months of Doxycycline, repeat endoscopy and biopsies confirmed resolution.
Discussion: WD disproportionally affects middle-age Caucasian males in an 8:1 male-female ratio. Annual incidence is ~3 per 1 million people. Mean time from first symptom onset to diagnosis is 7 years. WD is fatal if unrecognized or untreated. Soil exposure and genetic predisposition are potential risk factors. Diagnosis is made with non-invasive PCR testing and duodenal biopsy for PCR and histopathology. The prodromal stage of WD is characterized by arthralgia/arthritis and precedes GI symptoms by years. The subsequent steady-state stage consists of diarrhea, weight loss and extraintestinal manifestations, such as neurologic and cardiac symptoms. Dermatologic findings are rare and variable.
Treatment results in rapid symptomatic improvement, but bacterial eradication requires prolonged therapy. Two weeks of ceftriaxone followed by 1 year of TMP-SMX is recommended. Tetracyclines are an alternative, but reports suggest higher risk of relapse. Duodenal biopsy should be repeated at 6-month intervals and therapy continued until biopsy is negative.
Disclosures:
Vivek V. Jasti, MD1, Jessica Barrett, DO2, Marty M. Meyer, MD3, Jessica A.. Hemminger, MD4, Shail Govani, MD, MSc5. P2699 - Whipple's Disease with Dermatologic Manifestations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2OhioHealth, Columbus, OH; 3Ohio Gastroenterology Group, Inc., Dublin, OH; 4Mount Carmel Health System, Columbus, OH; 5Ohio Gastroenterology Group, Inc., Columbus, OH
Introduction: Whipple’s disease (WD) is a rare, chronic infection due to Tropheryma whipplei (TW). Symptoms are non-specific and progress slowly. We present a case of WD with abnormal skin findings.
Case Description/Methods: A 72-year-old Caucasian female with a 2-year history of migratory polyarthritis presented for workup of chronic diarrhea, iron deficiency anemia, and 30lb weight loss over 7 months. Recent upper endoscopy and colonoscopy for anemia was unremarkable. Capsule endoscopy revealed jejunal lymphangiectasias. Follow up push enteroscopy showed diffuse dilated lacteals and villous blunting. Duodenal and jejunal mucosal biopsies contained an extensive infiltrate of PAS-positive foamy macrophages in the lamina propria. TW PCR was positive, confirming WD. Inpatient admission was arranged, at which time new lower extremity erythema and edema was noted. Punch biopsy of the skin lesion also revealed PAS-positive macrophages. Skin and blood were TW PCR positive. Lumbar puncture was performed; CSF PCR was negative. Treatment was started with IV ceftriaxone 2g daily for 2 weeks followed by trimethoprim-sulfamethoxazole (TMP-SMX). After 3 weeks the patient reported symptomatic and dermatologic improvement. Due to asymptomatic alkaline phosphatase elevation, TMP-SMX was changed to doxycycline after 7 months. Repeat endoscopy and biopsy at 7 and 12 months revealed active disease. After 9 more months of Doxycycline, repeat endoscopy and biopsies confirmed resolution.
Discussion: WD disproportionally affects middle-age Caucasian males in an 8:1 male-female ratio. Annual incidence is ~3 per 1 million people. Mean time from first symptom onset to diagnosis is 7 years. WD is fatal if unrecognized or untreated. Soil exposure and genetic predisposition are potential risk factors. Diagnosis is made with non-invasive PCR testing and duodenal biopsy for PCR and histopathology. The prodromal stage of WD is characterized by arthralgia/arthritis and precedes GI symptoms by years. The subsequent steady-state stage consists of diarrhea, weight loss and extraintestinal manifestations, such as neurologic and cardiac symptoms. Dermatologic findings are rare and variable.
Treatment results in rapid symptomatic improvement, but bacterial eradication requires prolonged therapy. Two weeks of ceftriaxone followed by 1 year of TMP-SMX is recommended. Tetracyclines are an alternative, but reports suggest higher risk of relapse. Duodenal biopsy should be repeated at 6-month intervals and therapy continued until biopsy is negative.
Disclosures:
Vivek Jasti indicated no relevant financial relationships.
Jessica Barrett indicated no relevant financial relationships.
Marty Meyer indicated no relevant financial relationships.
Jessica Hemminger indicated no relevant financial relationships.
Shail Govani: Abbvie – Advisory Committee/Board Member, Speakers Bureau. Bristol Meyers Squibb – Speakers Bureau.
Vivek V. Jasti, MD1, Jessica Barrett, DO2, Marty M. Meyer, MD3, Jessica A.. Hemminger, MD4, Shail Govani, MD, MSc5. P2699 - Whipple's Disease with Dermatologic Manifestations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
