Monday Poster Session
Category: Small Intestine
P2704 - The Great Squeeze: When Histoplasmosis Turns Your Bowels into a Twisted Maze!
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- BD
Brett A. Dinner, MD
Creighton University
Phoenix, AZ
Presenting Author(s)
Brett A. Dinner, MD1, Ericka Charley, MD2, Phillip Leff, DO1, Matthew M. Barvo, MD1, Robert Lee, MD1, Keng-Yu Chuang, MD3
1Creighton University, Phoenix, AZ; 2Creighton University Phoenix, Mesa, AZ; 3Valleywise Health, Phoenix, AZ
Introduction: Histoplasmosis is a systemic endemic fungal infection. Pulmonary histoplasmosis is generally a benign disease in immunocompetent patients. In severe cases or in immunocompromised individuals, the infection can spread beyond the lungs to other organs including the liver, spleen, lymph nodes (LN), bone marrow, and gastrointestinal (GI) tract mucosa. Herein, we present a case of disseminated histoplasmosis (DH) leading to severe mesenteric lymphadenitis and subsequent small bowel obstruction (SBO).
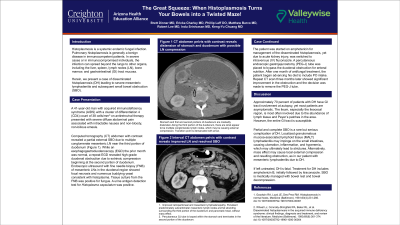
Case Description/Methods: A 41-year-old man with AIDS with a CD4 count of 38 on antiretroviral therapy presented with severe diffuse abdominal pain associated with intractable nausea and nonbloody, nonbilious emesis. CT abdomen with contrast revealed a partial external SBO due to multiple conglomerate mesenteric LN near the third portion of duodenum (Figure 1). While an esophagogastroduodenoscopy (EGD) the prior month was normal, a repeat EGD revealed high-grade duodenal obstruction due to extrinsic compression beginning at the second portion of duodenum. Fine needle biopsies (FNB) of mesenteric LN in the duodenal region showed focal necrosis and numerous buddying yeast consistent with histoplasma. Tissue culture from the FNB was positive for fungus. A urine antigen detection test for Histoplasma capsulatum was positive. For DH, the patient was started on amphotericin, yet due to AKI, was switched to fluconazole IV. A PEG-J tube was placed to bypass the duodenal obstruction for enteral nutrition. After one month of antifungal treatment, the patient began advancing his diet to include PO intake.
Discussion: Approximately 70 percent of patients with DH have GI tract involvement at autopsy, yet most patients are asymptomatic. The ileum, especially the ileocecal area, is most often involved, due to the abundance of lymph tissue and Peyer’s patches. However, the entire GI tract is susceptible
Partial and complete SBO is a rare but serious complication of DH. Localized granulomatous mucosa-associated lymphoid tissue (MALT) lymphadenitis may impinge on small intestines, causing ulceration, inflammation and hyperemia, which may lead to strictures. Alternatively, mass effect may cause local external compression and resulting obstruction, as in our patient with mesenteric lymphadenitis due to DH.
If left untreated, DH is fatal. Treatment for DH includes amphotericin B initially followed by itraconazole. SBO is medically managed with bowel rest and bowel decompression.

Disclosures:
Brett A. Dinner, MD1, Ericka Charley, MD2, Phillip Leff, DO1, Matthew M. Barvo, MD1, Robert Lee, MD1, Keng-Yu Chuang, MD3. P2704 - The Great Squeeze: When Histoplasmosis Turns Your Bowels into a Twisted Maze!, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Creighton University, Phoenix, AZ; 2Creighton University Phoenix, Mesa, AZ; 3Valleywise Health, Phoenix, AZ
Introduction: Histoplasmosis is a systemic endemic fungal infection. Pulmonary histoplasmosis is generally a benign disease in immunocompetent patients. In severe cases or in immunocompromised individuals, the infection can spread beyond the lungs to other organs including the liver, spleen, lymph nodes (LN), bone marrow, and gastrointestinal (GI) tract mucosa. Herein, we present a case of disseminated histoplasmosis (DH) leading to severe mesenteric lymphadenitis and subsequent small bowel obstruction (SBO).
Case Description/Methods: A 41-year-old man with AIDS with a CD4 count of 38 on antiretroviral therapy presented with severe diffuse abdominal pain associated with intractable nausea and nonbloody, nonbilious emesis. CT abdomen with contrast revealed a partial external SBO due to multiple conglomerate mesenteric LN near the third portion of duodenum (Figure 1). While an esophagogastroduodenoscopy (EGD) the prior month was normal, a repeat EGD revealed high-grade duodenal obstruction due to extrinsic compression beginning at the second portion of duodenum. Fine needle biopsies (FNB) of mesenteric LN in the duodenal region showed focal necrosis and numerous buddying yeast consistent with histoplasma. Tissue culture from the FNB was positive for fungus. A urine antigen detection test for Histoplasma capsulatum was positive. For DH, the patient was started on amphotericin, yet due to AKI, was switched to fluconazole IV. A PEG-J tube was placed to bypass the duodenal obstruction for enteral nutrition. After one month of antifungal treatment, the patient began advancing his diet to include PO intake.
Discussion: Approximately 70 percent of patients with DH have GI tract involvement at autopsy, yet most patients are asymptomatic. The ileum, especially the ileocecal area, is most often involved, due to the abundance of lymph tissue and Peyer’s patches. However, the entire GI tract is susceptible
Partial and complete SBO is a rare but serious complication of DH. Localized granulomatous mucosa-associated lymphoid tissue (MALT) lymphadenitis may impinge on small intestines, causing ulceration, inflammation and hyperemia, which may lead to strictures. Alternatively, mass effect may cause local external compression and resulting obstruction, as in our patient with mesenteric lymphadenitis due to DH.
If left untreated, DH is fatal. Treatment for DH includes amphotericin B initially followed by itraconazole. SBO is medically managed with bowel rest and bowel decompression.

Figure: Figure 1
Disclosures:
Brett Dinner indicated no relevant financial relationships.
Ericka Charley indicated no relevant financial relationships.
Phillip Leff indicated no relevant financial relationships.
Matthew Barvo indicated no relevant financial relationships.
Robert Lee indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Brett A. Dinner, MD1, Ericka Charley, MD2, Phillip Leff, DO1, Matthew M. Barvo, MD1, Robert Lee, MD1, Keng-Yu Chuang, MD3. P2704 - The Great Squeeze: When Histoplasmosis Turns Your Bowels into a Twisted Maze!, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
