Monday Poster Session
Category: Stomach
P2715 - Optimizing Surveillance Strategies for Gastric Cancer in Lynch Syndrome: A Cost-Effectiveness Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- JY
Ji Yoon Yoon, MD, MSCR
Icahn School of Medicine at Mount Sinai
New York, New York
Presenting Author(s)
Award: ACG Auxiliary Award (Trainee)
Award: Presidential Poster Award
Ji Yoon Yoon, MD, MSCR1, Emily Leven, MD1, Chin Hur, MD, MPH2, Carol A. Burke, MD, FACG3, Aimee Lucas, MD, MS1
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Columbia University Irving Medical Center, New York, NY; 3Cleveland Clinic Foundation, Cleveland, OH
Introduction: Lynch syndrome (LS) is one of the most common hereditary colorectal cancer syndromes, caused by germline pathogenic variants (PV) in MLH1, MSH2/EPCAM, MSH6, PMS2. Gastric cancer risk in LS is up to 11%, varying by PV, versus 0.9% in the general population, and is the first LS spectrum cancer in 39% patients. Most LS gastric cancer have a precancerous (Correa) cascade amenable to endoscopic intervention. Guidelines recommend upper endoscopy (EGD) every 2-4 years starting age 30-40, performed at time of colonoscopy. We present a comparative effectiveness study of EGD surveillance for gastric cancer in LS by PV.
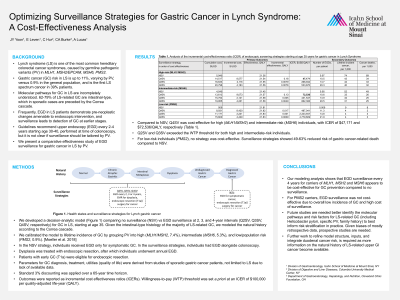
Methods: We developed a decision-analytic model comparing no surveillance (NSV) vs EGD surveillance at 2, 3, and 4-year intervals (Q2SV, Q3SV, Q4SV, respectively) for gastric cancer in LS, starting at age 35. In the NSV strategy, individuals received EGD only for symptomatic gastric cancer. In the surveillance strategies, individuals had EGD alongside colonoscopy. Dysplasia and early gastric cancer were treated with endoscopic resection (Figure 1). We calibrated the model to lifetime incidence of gastric cancer by grouping PV into high (MLH1/MSH2, 7.4%), intermediate (MSH6, 5.3%), and low/population risk (PMS2, 0.9%). Utilities measuring quality of life, costs and complication rates of intervention were derived from literature. Standard 3% discounting was applied over a 65-year time horizon. Outcomes were reported as incremental cost effectiveness ratios (ICERs). Willingness-to-pay (WTP) threshold was set a priori at an ICER of $100,000 per quality-adjusted life-year (QALY).
Results: Compared to NSV, Q4SV was cost-effective for high (MLH1/MSH2) and intermediate-risk (MSH6) individuals, with ICER of $47,171 and $72,536/QALY, respectively (Table 1). Q2SV and Q3SV exceeded the WTP threshold for both high and intermediate-risk individuals. For low-risk individuals (PMS2), no strategy was cost-effective. Surveillance strategies showed 49-63% reduced risk of gastric cancer-related death compared to NSV.
Discussion: Our modeling analysis shows that EGD surveillance every 4 years for carriers of MLH1, MSH2 and MSH6 appears to be cost-effective for gastric cancer prevention. For PMS2 carriers, EGD surveillance was not cost-effective. Future studies are needed to better understand the risk of gastric and small bowel cancer in LS and identify the risk factors (including Helicobacter pylori, specific PV, family history) to best inform risk stratification in practice.

Disclosures:
Ji Yoon Yoon, MD, MSCR1, Emily Leven, MD1, Chin Hur, MD, MPH2, Carol A. Burke, MD, FACG3, Aimee Lucas, MD, MS1. P2715 - Optimizing Surveillance Strategies for Gastric Cancer in Lynch Syndrome: A Cost-Effectiveness Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Award: Presidential Poster Award
Ji Yoon Yoon, MD, MSCR1, Emily Leven, MD1, Chin Hur, MD, MPH2, Carol A. Burke, MD, FACG3, Aimee Lucas, MD, MS1
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Columbia University Irving Medical Center, New York, NY; 3Cleveland Clinic Foundation, Cleveland, OH
Introduction: Lynch syndrome (LS) is one of the most common hereditary colorectal cancer syndromes, caused by germline pathogenic variants (PV) in MLH1, MSH2/EPCAM, MSH6, PMS2. Gastric cancer risk in LS is up to 11%, varying by PV, versus 0.9% in the general population, and is the first LS spectrum cancer in 39% patients. Most LS gastric cancer have a precancerous (Correa) cascade amenable to endoscopic intervention. Guidelines recommend upper endoscopy (EGD) every 2-4 years starting age 30-40, performed at time of colonoscopy. We present a comparative effectiveness study of EGD surveillance for gastric cancer in LS by PV.
Methods: We developed a decision-analytic model comparing no surveillance (NSV) vs EGD surveillance at 2, 3, and 4-year intervals (Q2SV, Q3SV, Q4SV, respectively) for gastric cancer in LS, starting at age 35. In the NSV strategy, individuals received EGD only for symptomatic gastric cancer. In the surveillance strategies, individuals had EGD alongside colonoscopy. Dysplasia and early gastric cancer were treated with endoscopic resection (Figure 1). We calibrated the model to lifetime incidence of gastric cancer by grouping PV into high (MLH1/MSH2, 7.4%), intermediate (MSH6, 5.3%), and low/population risk (PMS2, 0.9%). Utilities measuring quality of life, costs and complication rates of intervention were derived from literature. Standard 3% discounting was applied over a 65-year time horizon. Outcomes were reported as incremental cost effectiveness ratios (ICERs). Willingness-to-pay (WTP) threshold was set a priori at an ICER of $100,000 per quality-adjusted life-year (QALY).
Results: Compared to NSV, Q4SV was cost-effective for high (MLH1/MSH2) and intermediate-risk (MSH6) individuals, with ICER of $47,171 and $72,536/QALY, respectively (Table 1). Q2SV and Q3SV exceeded the WTP threshold for both high and intermediate-risk individuals. For low-risk individuals (PMS2), no strategy was cost-effective. Surveillance strategies showed 49-63% reduced risk of gastric cancer-related death compared to NSV.
Discussion: Our modeling analysis shows that EGD surveillance every 4 years for carriers of MLH1, MSH2 and MSH6 appears to be cost-effective for gastric cancer prevention. For PMS2 carriers, EGD surveillance was not cost-effective. Future studies are needed to better understand the risk of gastric and small bowel cancer in LS and identify the risk factors (including Helicobacter pylori, specific PV, family history) to best inform risk stratification in practice.

Figure: Figure 1. Schematic of strategies for Lynch Syndrome cohort
Q2SV, Q3SV, Q4SV: EGD surveillance every 2, 3, or 4 years, respectively. If gastric dysplasia, endoscopic resection followed by endoscopic surveillance per current guidelines for gastric dysplasia. NSV: endoscopy for symptomatic cancer only. In all surveillance strategies, early cancer (T1a) had endoscopic resection; more advanced cancers had surgery.
Q2SV, Q3SV, Q4SV: EGD surveillance every 2, 3, or 4 years, respectively. If gastric dysplasia, endoscopic resection followed by endoscopic surveillance per current guidelines for gastric dysplasia. NSV: endoscopy for symptomatic cancer only. In all surveillance strategies, early cancer (T1a) had endoscopic resection; more advanced cancers had surgery.
Disclosures:
Ji Yoon Yoon indicated no relevant financial relationships.
Emily Leven indicated no relevant financial relationships.
Chin Hur: Exact Sciences – Consultant. Vivante – Stock Options.
Carol Burke: ambry – Speakers Bureau. emtora – Grant/Research Support. freenome – Grant/Research Support. guardant – Advisory Committee/Board Member. sebela – Consultant.
Aimee Lucas: AiOnco – Consultant, Grant/Research Support. ClearNote Health – Advisor or Review Panel Member. Immunovia – Consultant, Grant/Research Support.
Ji Yoon Yoon, MD, MSCR1, Emily Leven, MD1, Chin Hur, MD, MPH2, Carol A. Burke, MD, FACG3, Aimee Lucas, MD, MS1. P2715 - Optimizing Surveillance Strategies for Gastric Cancer in Lynch Syndrome: A Cost-Effectiveness Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

