Monday Poster Session
Category: Stomach
P2719 - Evaluating the Impact of a Dedicated Gastric Biopsy Clinic Visit on Gastric Intestinal Metaplasia Surveillance Compliance
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- JK
Jennifer Koh, MD, MPH
Keck School of Medicine of USC
Los Angeles, California
Presenting Author(s)
Award: Presidential Poster Award
Jennifer Koh, MD, MPH1, Denis Nguyen, MD1, Sarah Wang, MD, MPH1, Nisha Sharma, MD1, Helen Lee, NP2, James Buxbaum, MD, MS1
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Gastric cancer is a leading cause of cancer death. The ability to identify precursor lesions including gastric intestinal metaplasia (GIM) has fostered interest in endoscopic surveillance. American societies now recommend surveillance endoscopy among those with GIM and demographic risk factors. We aim to gauge the compliance of surveillance endoscopies after the initiation of a dedicated post endoscopy visit to discuss GIM.
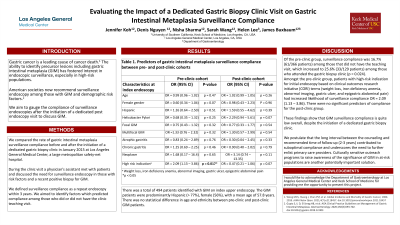
Methods: We compared the rate of surveillance compliance before and after the initiation of a dedicated gastric biopsy clinic in January 2015 at Los Angeles General Medical Center, a safety-net hospital. During the clinic visit a physician’s assistant met with patients and discussed the need for surveillance in those with risk factors and a recent positive biopsy for GIM. We defined surveillance compliance as a repeat endoscopy within 3 years. We aimed to identify factors which predicted compliance among those who did or did not have the clinic teaching visit.
Results: There was a total of 494 patients identified with GIM on index upper endoscopy. The GIM patients were predominantly female (56%), Hispanic ( >77%), with a mean age of 57.8 years.
There was no statistical difference in age and ethnicity between pre-clinic and post-clinic GIM patients. Of the pre-clinic group, surveillance compliance was 16.7% (61/366 patients) among those that did not have the teaching visit, which increased to 25.6% (33/129 patients) among those who attended the gastric biopsy clinic (p = 0.024).
Amongst the pre-clinic group, patients with high-risk indication for initial endoscopy based on clinical outcomes research initiative (CORI) terms (weight loss, iron deficiency anemia, abnormal imaging, gastric ulcer, and epigastric abdominal pain) had increased likelihood of surveillance compliance OR = 2.09 (1.13 – 3.86). There were no significant predictors of compliance for the post-clinic group.
Discussion: These findings show that GIM surveillance compliance is quite low overall, despite the initiation of a dedicated gastric biopsy clinic. We postulate that the long interval between the counseling and recommended time of follow-up (2-3 years) contributed to suboptimal compliance and underscores the need to further enlist primary care providers. Culturally sensitive outreach programs to raise awareness of the significance of GIM in at-risk populations are another potentially important solution.
Disclosures:
Jennifer Koh, MD, MPH1, Denis Nguyen, MD1, Sarah Wang, MD, MPH1, Nisha Sharma, MD1, Helen Lee, NP2, James Buxbaum, MD, MS1. P2719 - Evaluating the Impact of a Dedicated Gastric Biopsy Clinic Visit on Gastric Intestinal Metaplasia Surveillance Compliance, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Jennifer Koh, MD, MPH1, Denis Nguyen, MD1, Sarah Wang, MD, MPH1, Nisha Sharma, MD1, Helen Lee, NP2, James Buxbaum, MD, MS1
1Keck School of Medicine of USC, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Gastric cancer is a leading cause of cancer death. The ability to identify precursor lesions including gastric intestinal metaplasia (GIM) has fostered interest in endoscopic surveillance. American societies now recommend surveillance endoscopy among those with GIM and demographic risk factors. We aim to gauge the compliance of surveillance endoscopies after the initiation of a dedicated post endoscopy visit to discuss GIM.
Methods: We compared the rate of surveillance compliance before and after the initiation of a dedicated gastric biopsy clinic in January 2015 at Los Angeles General Medical Center, a safety-net hospital. During the clinic visit a physician’s assistant met with patients and discussed the need for surveillance in those with risk factors and a recent positive biopsy for GIM. We defined surveillance compliance as a repeat endoscopy within 3 years. We aimed to identify factors which predicted compliance among those who did or did not have the clinic teaching visit.
Results: There was a total of 494 patients identified with GIM on index upper endoscopy. The GIM patients were predominantly female (56%), Hispanic ( >77%), with a mean age of 57.8 years.
There was no statistical difference in age and ethnicity between pre-clinic and post-clinic GIM patients. Of the pre-clinic group, surveillance compliance was 16.7% (61/366 patients) among those that did not have the teaching visit, which increased to 25.6% (33/129 patients) among those who attended the gastric biopsy clinic (p = 0.024).
Amongst the pre-clinic group, patients with high-risk indication for initial endoscopy based on clinical outcomes research initiative (CORI) terms (weight loss, iron deficiency anemia, abnormal imaging, gastric ulcer, and epigastric abdominal pain) had increased likelihood of surveillance compliance OR = 2.09 (1.13 – 3.86). There were no significant predictors of compliance for the post-clinic group.
Discussion: These findings show that GIM surveillance compliance is quite low overall, despite the initiation of a dedicated gastric biopsy clinic. We postulate that the long interval between the counseling and recommended time of follow-up (2-3 years) contributed to suboptimal compliance and underscores the need to further enlist primary care providers. Culturally sensitive outreach programs to raise awareness of the significance of GIM in at-risk populations are another potentially important solution.
Disclosures:
Jennifer Koh indicated no relevant financial relationships.
Denis Nguyen indicated no relevant financial relationships.
Sarah Wang indicated no relevant financial relationships.
Nisha Sharma indicated no relevant financial relationships.
Helen Lee indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
Jennifer Koh, MD, MPH1, Denis Nguyen, MD1, Sarah Wang, MD, MPH1, Nisha Sharma, MD1, Helen Lee, NP2, James Buxbaum, MD, MS1. P2719 - Evaluating the Impact of a Dedicated Gastric Biopsy Clinic Visit on Gastric Intestinal Metaplasia Surveillance Compliance, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

