Monday Poster Session
Category: Stomach
P2733 - Diagnostic Performance of Blue Laser Imaging for Gastric Cancer: A Systematic Review and Meta-analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- MS
Mohammed Rifat Shaik, MBBS
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS1, Shivanand Bomman, MD2, Andrew Canakis, DO3
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Arizona School of Medicine, Tucson, AZ; 3University of Maryland Medical Center, Baltimore, MD
Introduction: Gastric cancer (GC) ranks as the third leading cause of cancer-related mortality worldwide, underscoring the urgent need for early detection strategies to improve survival rates. While esophagogastroduodenoscopy (EGD) with conventional white-light imaging (C-WLI) is a highly effective method for detecting early GC, it has been reported to miss 19-26% of cases. In light of these limitations, we aimed to conduct a comprehensive meta-analysis to evaluate the diagnostic performance of Blue Laser Imaging (BLI) in the detection of GC.
Methods: Various databases were searched to identify studies that utilized BLI for detecting GC. Two independent reviewers screened the titles/abstracts and conducted a full-text review of the studies. Genetic variance inverse effects model was employed to derive the event rates along with 95% confidence intervals (CI). The QUADS-2 tool was used to evaluate diagnostic accuracy and potential bias in the included studies. Our primary objectives were to assess the sensitivity, specificity, and accuracy of BLI in GC detection.
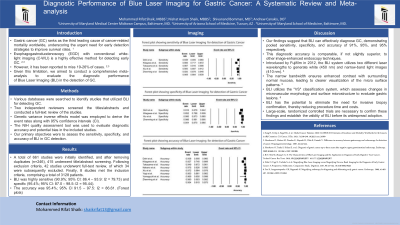
Results: A total of 661 studies were initially identified, and after removing duplicates (n=246), 415 underwent title/abstract screening. Following exclusion criteria, 42 studies underwent full-text review, of which 34 were subsequently excluded. Finally, 8 studies met the inclusion criteria, comprising a total of 3128 patients (Flowchart). BLI was highly sensitive (90.9%; 95% CI: 86.4 – 93.9: I2 = 79.73) and specific (95.4%; 95% CI: 87.0 – 98.5: I2 = 95.44). The accuracy was 95.4%; 95% CI 91.5 – 97.5: I2 = 86.61. (Forest plots)
Discussion: Our findings suggest that BLI can effectively diagnose GC, demonstrating pooled sensitivity, specificity, and accuracy of 91%, 95%, and 95% respectively. This diagnostic accuracy is comparable, if not slightly superior, to other image-enhanced endoscopy techniques. BLI utilizes the "VS" classification system, which assesses changes in microvascular morphology and surface microstructure to evaluate gastric lesions. By combining narrow-band laser light with illumination light, BLI enhances brightness, enabling clearer and more detailed observations of lesion characteristics. BLI has the potential to eliminate the need for invasive biopsy confirmation, thereby reducing procedure time and costs. Nevertheless, large-scale, randomized controlled trials are necessary to confirm these findings and establish the validity of BLI before its widespread adoption.

Disclosures:
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS1, Shivanand Bomman, MD2, Andrew Canakis, DO3. P2733 - Diagnostic Performance of Blue Laser Imaging for Gastric Cancer: A Systematic Review and Meta-analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Arizona School of Medicine, Tucson, AZ; 3University of Maryland Medical Center, Baltimore, MD
Introduction: Gastric cancer (GC) ranks as the third leading cause of cancer-related mortality worldwide, underscoring the urgent need for early detection strategies to improve survival rates. While esophagogastroduodenoscopy (EGD) with conventional white-light imaging (C-WLI) is a highly effective method for detecting early GC, it has been reported to miss 19-26% of cases. In light of these limitations, we aimed to conduct a comprehensive meta-analysis to evaluate the diagnostic performance of Blue Laser Imaging (BLI) in the detection of GC.
Methods: Various databases were searched to identify studies that utilized BLI for detecting GC. Two independent reviewers screened the titles/abstracts and conducted a full-text review of the studies. Genetic variance inverse effects model was employed to derive the event rates along with 95% confidence intervals (CI). The QUADS-2 tool was used to evaluate diagnostic accuracy and potential bias in the included studies. Our primary objectives were to assess the sensitivity, specificity, and accuracy of BLI in GC detection.
Results: A total of 661 studies were initially identified, and after removing duplicates (n=246), 415 underwent title/abstract screening. Following exclusion criteria, 42 studies underwent full-text review, of which 34 were subsequently excluded. Finally, 8 studies met the inclusion criteria, comprising a total of 3128 patients (Flowchart). BLI was highly sensitive (90.9%; 95% CI: 86.4 – 93.9: I2 = 79.73) and specific (95.4%; 95% CI: 87.0 – 98.5: I2 = 95.44). The accuracy was 95.4%; 95% CI 91.5 – 97.5: I2 = 86.61. (Forest plots)
Discussion: Our findings suggest that BLI can effectively diagnose GC, demonstrating pooled sensitivity, specificity, and accuracy of 91%, 95%, and 95% respectively. This diagnostic accuracy is comparable, if not slightly superior, to other image-enhanced endoscopy techniques. BLI utilizes the "VS" classification system, which assesses changes in microvascular morphology and surface microstructure to evaluate gastric lesions. By combining narrow-band laser light with illumination light, BLI enhances brightness, enabling clearer and more detailed observations of lesion characteristics. BLI has the potential to eliminate the need for invasive biopsy confirmation, thereby reducing procedure time and costs. Nevertheless, large-scale, randomized controlled trials are necessary to confirm these findings and establish the validity of BLI before its widespread adoption.

Figure: Flow chart (left) represents the study protocol. Forest plots (right) demonstrate the pooled sensitivity, specificity and accuracy of Blue Laser Imaging in Gastric Cancer detection
Disclosures:
Mohammed Rifat Shaik indicated no relevant financial relationships.
Nishat Anjum Shaik indicated no relevant financial relationships.
Shivanand Bomman indicated no relevant financial relationships.
Andrew Canakis indicated no relevant financial relationships.
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS1, Shivanand Bomman, MD2, Andrew Canakis, DO3. P2733 - Diagnostic Performance of Blue Laser Imaging for Gastric Cancer: A Systematic Review and Meta-analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
