Monday Poster Session
Category: Stomach
P2734 - Communication and Surveillance Recommendations on Gastric Intestinal Metaplasia by US Gastroenterologists Before and After the 2020 American Gastroenterological Association Guidelines: Data From a Tertiary Care Center
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Baila Elkin, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Baila Elkin, MD1, Joseph El Dahdah, MD2, Qijun Yang, MS3, Michelle Kim, MD1, Shailja C. Shah, MD, MPH4, Carol Rouphael, MD2
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Lerner Research Institute, Cleveland, OH; 4Jennifer Moreno Veteran Affairs San Diego Healthcare System, San Diego, CA
Introduction: Gastric intestinal metaplasia (GIM) is a precursor to non-cardia gastric cancer (NCGC). Studies showed variability in gastroenterologists’ (GE) knowledge and management of GIM, attributed to limited guidance from US GI societies. In 2020, the American Gastroenterological Association (AGA) published GIM guidelines, recommending against routine surveillance and advising physician/patient shared decision-making on surveillance based on risk factors. We hypothesize awareness of risk factors for GIM progression and surveillance recommendations have increased since the guidelines. We hence sought to compare GE’s communication trends of GIM finding as well as surveillance recommendations before and after 2020 at a tertiary care center.
Methods: A sample of patients with GIM on biopsies from upper endoscopies (EGD) performed between 1/2018 and 12/2022 were included in this retrospective cohort study. Exclusions were history of gastric cancer or surgery, cardia-only GIM and hereditary cancer syndromes. Cohort A included GIM patients diagnosed < 2020 and cohort B >2020. Data were manually collected from the electronic medical record. GEs’ communication of a GIM finding was deemed present if there was a communication about GIM via phone, MyChart, letter, office visit or other. Mapping recommendation to determine GIM extent was defined if repeat endoscopy was recommended within 1 year of baseline EGD and surveillance recommendation if EGD advised >1 year. Pearson's Chi-square and Fisher’s exact tests were used for categorical variables and Wilcoxon rank sum test for continuous variables. Analyses were performed with R software.
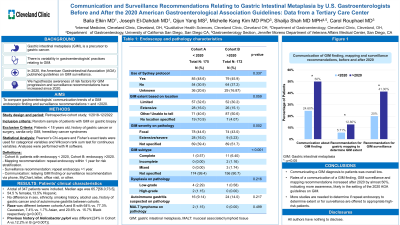
Results: 347 patients were included: 175 in cohort A and 172 in cohort B. Median age was 65.7 [56.0, 73.4] and 54.5% were females. Patients’ demographic, clinical, endoscopic and pathology characteristics are presented in Table 1. GEs’ communication to patients about GIM finding increased from 24.6% < 2020 to 50% >2020 (p< 0.001). Similarly, there was a significant increase in mapping and surveillance recommendations after 2020 (5.71% vs 12.8%, p=0.036 and 41.3% >2020 vs 20% < 2020, p< 0.001 respectively) (Figure 1).
Discussion: While communicating a GIM diagnosis to patients was overall low, the rates of communication, surveillance and mapping recommendations increased after 2020, indicating more awareness, likely in the setting of the 2020 AGA guidelines on GIM. More studies are needed to determine if mapping and surveillance are offered to appropriate high-risk patients.

Disclosures:
Baila Elkin, MD1, Joseph El Dahdah, MD2, Qijun Yang, MS3, Michelle Kim, MD1, Shailja C. Shah, MD, MPH4, Carol Rouphael, MD2. P2734 - Communication and Surveillance Recommendations on Gastric Intestinal Metaplasia by US Gastroenterologists Before and After the 2020 American Gastroenterological Association Guidelines: Data From a Tertiary Care Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Lerner Research Institute, Cleveland, OH; 4Jennifer Moreno Veteran Affairs San Diego Healthcare System, San Diego, CA
Introduction: Gastric intestinal metaplasia (GIM) is a precursor to non-cardia gastric cancer (NCGC). Studies showed variability in gastroenterologists’ (GE) knowledge and management of GIM, attributed to limited guidance from US GI societies. In 2020, the American Gastroenterological Association (AGA) published GIM guidelines, recommending against routine surveillance and advising physician/patient shared decision-making on surveillance based on risk factors. We hypothesize awareness of risk factors for GIM progression and surveillance recommendations have increased since the guidelines. We hence sought to compare GE’s communication trends of GIM finding as well as surveillance recommendations before and after 2020 at a tertiary care center.
Methods: A sample of patients with GIM on biopsies from upper endoscopies (EGD) performed between 1/2018 and 12/2022 were included in this retrospective cohort study. Exclusions were history of gastric cancer or surgery, cardia-only GIM and hereditary cancer syndromes. Cohort A included GIM patients diagnosed < 2020 and cohort B >2020. Data were manually collected from the electronic medical record. GEs’ communication of a GIM finding was deemed present if there was a communication about GIM via phone, MyChart, letter, office visit or other. Mapping recommendation to determine GIM extent was defined if repeat endoscopy was recommended within 1 year of baseline EGD and surveillance recommendation if EGD advised >1 year. Pearson's Chi-square and Fisher’s exact tests were used for categorical variables and Wilcoxon rank sum test for continuous variables. Analyses were performed with R software.
Results: 347 patients were included: 175 in cohort A and 172 in cohort B. Median age was 65.7 [56.0, 73.4] and 54.5% were females. Patients’ demographic, clinical, endoscopic and pathology characteristics are presented in Table 1. GEs’ communication to patients about GIM finding increased from 24.6% < 2020 to 50% >2020 (p< 0.001). Similarly, there was a significant increase in mapping and surveillance recommendations after 2020 (5.71% vs 12.8%, p=0.036 and 41.3% >2020 vs 20% < 2020, p< 0.001 respectively) (Figure 1).
Discussion: While communicating a GIM diagnosis to patients was overall low, the rates of communication, surveillance and mapping recommendations increased after 2020, indicating more awareness, likely in the setting of the 2020 AGA guidelines on GIM. More studies are needed to determine if mapping and surveillance are offered to appropriate high-risk patients.

Figure: Figure 1: Communication about GIM finding, mapping and surveillance recommendations before and after 2020
GIM: Gastric Intestinal Metaplasia
GIM: Gastric Intestinal Metaplasia
Disclosures:
Baila Elkin indicated no relevant financial relationships.
Joseph El Dahdah indicated no relevant financial relationships.
Qijun Yang indicated no relevant financial relationships.
Michelle Kim indicated no relevant financial relationships.
Shailja Shah: GLG – Consultant. Guidepoint – Consultant. Phathom Pharmaceuticals – Consultant. RedHill Biopharma – Consultant.
Carol Rouphael indicated no relevant financial relationships.
Baila Elkin, MD1, Joseph El Dahdah, MD2, Qijun Yang, MS3, Michelle Kim, MD1, Shailja C. Shah, MD, MPH4, Carol Rouphael, MD2. P2734 - Communication and Surveillance Recommendations on Gastric Intestinal Metaplasia by US Gastroenterologists Before and After the 2020 American Gastroenterological Association Guidelines: Data From a Tertiary Care Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
