Monday Poster Session
Category: Stomach
P2737 - Repeated Measurements Provide Consistent Categorization of Delayed Emptying Among Patients With Gastroparesis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Ting Zheng, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Michael Camilleri, MD, DSc, Ting Zheng, MD, Ann Taylor, CCRC, Saam Dilmaghani, MD, MPH, Joelle BouSaba, MD, Michael Ryks, , Irene Busciglio, , Duane D. Burton, MA
Mayo Clinic, Rochester, MN
Introduction: The intra individual coefficients of variation (COV) in gastric emptying (GE) of solids in patients with functional dyspepsia (FD) and with gastroparesis (Gp) has resulted in the perception of overlap between the 2 syndromes. We hypothesized that, among participants given a previously validated high-calorie and high-fat content solid radiolabeled meal, intra-individual COV in GE parameters over time would not impact patients’ classification as normal or delayed GE. Our aim was to estimate variation of time to achieve 50% GE (GET1/2), as well as GE at 2 and 4 hours among patients with gastroparesis over a 4-week period.
Methods: We evaluated the data previously obtained in randomized, blinded, placebo-controlled trial of cannabidiol (DK122280). All patients had documented GE delay in medical records based on the same GE meal. We evaluated only those participants in the placebo arm who had baseline and 4-week GE measurements (21/23 total participants). The GE test meal was 320 kilocalorie, 30% fat consisting of 2 scrambled eggs, bread and milk. Statistical analysis compared data obtained at baseline and end of treatment in the placebo group. Bland-Altman plots were used to assess the range of the bias in the confidence interval of each measurement summarizing GE. McNemar’s Test and Cohen’s kappa was conducted to compare agreement of GE test results over time.
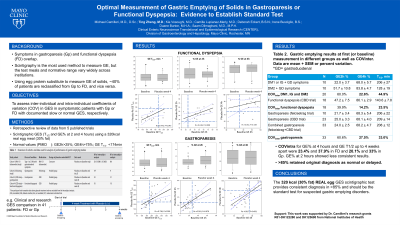
Results: 21 patients with gastroparesis (19 female, 71% idiopathic, 29% diabetic) were assessed at baseline and at end of 4 weeks treatment with placebo. Median BMI was 27.3 kg/m2 (10-90%ile 21.0 to 34.5 kg/m2) and age 44 y (range 22 to 61 y). The Table documents the small mean variations for 3 parameters in the 2 measurements among the 21 patients. Figure shows the linear regression plots for GET1/2, and percent emptied at 2 and 4 hours. In general, although there is variation, patients with abnormal GET1/2 remained abnormal ( >174 minutes, 95% of 314 normals [PMID 22747676]) on both studies. Agreement between the baseline and follow up GE study was consistent with substantial to almost perfect agreement (Cohen’s kappa = 0.800, 95% CI 0.542 – 1.000). McNemar’s test was nonsignificant (p = 0.157), meaning there is no significant evidence that the baseline and follow-up GE tests differed substantially.
Discussion: The 320 kilocalorie 30% fat meal provides consistent information regarding retardation of gastric emptying in patients with gastroparesis studied on 2 occasions 4 weeks apart.

Disclosures:
Michael Camilleri, MD, DSc, Ting Zheng, MD, Ann Taylor, CCRC, Saam Dilmaghani, MD, MPH, Joelle BouSaba, MD, Michael Ryks, , Irene Busciglio, , Duane D. Burton, MA. P2737 - Repeated Measurements Provide Consistent Categorization of Delayed Emptying Among Patients With Gastroparesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: The intra individual coefficients of variation (COV) in gastric emptying (GE) of solids in patients with functional dyspepsia (FD) and with gastroparesis (Gp) has resulted in the perception of overlap between the 2 syndromes. We hypothesized that, among participants given a previously validated high-calorie and high-fat content solid radiolabeled meal, intra-individual COV in GE parameters over time would not impact patients’ classification as normal or delayed GE. Our aim was to estimate variation of time to achieve 50% GE (GET1/2), as well as GE at 2 and 4 hours among patients with gastroparesis over a 4-week period.
Methods: We evaluated the data previously obtained in randomized, blinded, placebo-controlled trial of cannabidiol (DK122280). All patients had documented GE delay in medical records based on the same GE meal. We evaluated only those participants in the placebo arm who had baseline and 4-week GE measurements (21/23 total participants). The GE test meal was 320 kilocalorie, 30% fat consisting of 2 scrambled eggs, bread and milk. Statistical analysis compared data obtained at baseline and end of treatment in the placebo group. Bland-Altman plots were used to assess the range of the bias in the confidence interval of each measurement summarizing GE. McNemar’s Test and Cohen’s kappa was conducted to compare agreement of GE test results over time.
Results: 21 patients with gastroparesis (19 female, 71% idiopathic, 29% diabetic) were assessed at baseline and at end of 4 weeks treatment with placebo. Median BMI was 27.3 kg/m2 (10-90%ile 21.0 to 34.5 kg/m2) and age 44 y (range 22 to 61 y). The Table documents the small mean variations for 3 parameters in the 2 measurements among the 21 patients. Figure shows the linear regression plots for GET1/2, and percent emptied at 2 and 4 hours. In general, although there is variation, patients with abnormal GET1/2 remained abnormal ( >174 minutes, 95% of 314 normals [PMID 22747676]) on both studies. Agreement between the baseline and follow up GE study was consistent with substantial to almost perfect agreement (Cohen’s kappa = 0.800, 95% CI 0.542 – 1.000). McNemar’s test was nonsignificant (p = 0.157), meaning there is no significant evidence that the baseline and follow-up GE tests differed substantially.
Discussion: The 320 kilocalorie 30% fat meal provides consistent information regarding retardation of gastric emptying in patients with gastroparesis studied on 2 occasions 4 weeks apart.

Figure: Linear regression with 95% confidence interval in repeat measurements of gastric emptying in patients with gastroparesis.
Disclosures:
Michael Camilleri: NGM Biopharmaceuticals – Grant/Research Support.
Ting Zheng indicated no relevant financial relationships.
Ann Taylor indicated no relevant financial relationships.
Saam Dilmaghani indicated no relevant financial relationships.
Joelle BouSaba indicated no relevant financial relationships.
Michael Ryks indicated no relevant financial relationships.
Irene Busciglio indicated no relevant financial relationships.
Duane Burton indicated no relevant financial relationships.
Michael Camilleri, MD, DSc, Ting Zheng, MD, Ann Taylor, CCRC, Saam Dilmaghani, MD, MPH, Joelle BouSaba, MD, Michael Ryks, , Irene Busciglio, , Duane D. Burton, MA. P2737 - Repeated Measurements Provide Consistent Categorization of Delayed Emptying Among Patients With Gastroparesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
