Monday Poster Session
Category: Stomach
P2775 - Management of a Rare Case of Gastric Neuroendocrine Tumor
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- HR
Harini Rathinamanickam, MD
SIU School of Medicine
Springfield, IL
Presenting Author(s)
Harini Rathinamanickam, MD
SIU School of Medicine, Springfield, IL
Introduction: Gastric neuroendocrine tumors (GNET) are rare accounting for < 1% of all gastric neoplasms. We present a 51 y/o woman who was noted to have an incidental GNET type 1 lesion during EGD for variceal screening. It was successfully removed by endoscopic mucosal resection (EMR).
Case Description/Methods: 51 y/o Caucasian woman with DM type 1, hypothyroidism, vitiligo, congenital solitary kidney, HTN, HLD, RA, and OSA presents for EGD for variceal screening due to newly diagnosed NASH-related cirrhosis. EGD didn’t reveal varices but showed multiple gastric polyps with fundic gland appearance. One of the gastric polyps was atypical with nodularity and measured 1 cm. It was removed by a hot snare. Pathology showed grade 1 well-differentiated GNET type 1 positive for synaptophysin and chromogranin. Biopsies of the stomach were consistent with atrophic gastritis. Intrinsic factor antibody (IFA) was negative. Gastrin=474 pg/ml and chromogranin A=225 ng/ml. B12 levels were normal but the patient was on B12 supplementation. DOTATATE scan revealed increased activity in the pancreatic head. She underwent EUS, which did not reveal a pancreatic lesion. EUS at the site of gastric polyp resection at 6 months revealed a 10 mm residual lesion originating from the submucosa with a depth of 3 mm. No lymph nodes were noted. It was completely removed by EMR using a band ligator and snare. Patient to f/u with oncology.
Discussion: GNETs are of 3 types. Type 1 GNET often occurs in elderly women and is typically associated with atrophic gastritis or pernicious anemia (PA). Hence workup for PA should be considered using IFA and B12 levels. IFA is less sensitive and may be negative in PA. Diagnosis of PA should be could be considered in such patients in the setting of other features such as macrocytosis, and hypersegmented neutrophils especially if not corrected with B12 supplementation. Type 2 GNET is associated with MEN-1 syndrome and type 3 is associated with atypical carcinoid syndrome.
Endoscopically type 1 GNETs are most commonly noted in the gastric body or the fundus while type 3 is noted in the antrum. Type 3 is the most aggressive GNET. Endoscopic resection is recommended for type 1 and 2 tumors less than 2 cm. Gastrectomy is required for type 3 GNETs. Endoscopic surveillance every 6-12 months for 3 years and annually thereafter is recommended. Our case highlights the varied role of gastroenterologists in the management of GNETs including diagnosis, staging, treatment, and surveillance.

Disclosures:
Harini Rathinamanickam, MD. P2775 - Management of a Rare Case of Gastric Neuroendocrine Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
SIU School of Medicine, Springfield, IL
Introduction: Gastric neuroendocrine tumors (GNET) are rare accounting for < 1% of all gastric neoplasms. We present a 51 y/o woman who was noted to have an incidental GNET type 1 lesion during EGD for variceal screening. It was successfully removed by endoscopic mucosal resection (EMR).
Case Description/Methods: 51 y/o Caucasian woman with DM type 1, hypothyroidism, vitiligo, congenital solitary kidney, HTN, HLD, RA, and OSA presents for EGD for variceal screening due to newly diagnosed NASH-related cirrhosis. EGD didn’t reveal varices but showed multiple gastric polyps with fundic gland appearance. One of the gastric polyps was atypical with nodularity and measured 1 cm. It was removed by a hot snare. Pathology showed grade 1 well-differentiated GNET type 1 positive for synaptophysin and chromogranin. Biopsies of the stomach were consistent with atrophic gastritis. Intrinsic factor antibody (IFA) was negative. Gastrin=474 pg/ml and chromogranin A=225 ng/ml. B12 levels were normal but the patient was on B12 supplementation. DOTATATE scan revealed increased activity in the pancreatic head. She underwent EUS, which did not reveal a pancreatic lesion. EUS at the site of gastric polyp resection at 6 months revealed a 10 mm residual lesion originating from the submucosa with a depth of 3 mm. No lymph nodes were noted. It was completely removed by EMR using a band ligator and snare. Patient to f/u with oncology.
Discussion: GNETs are of 3 types. Type 1 GNET often occurs in elderly women and is typically associated with atrophic gastritis or pernicious anemia (PA). Hence workup for PA should be considered using IFA and B12 levels. IFA is less sensitive and may be negative in PA. Diagnosis of PA should be could be considered in such patients in the setting of other features such as macrocytosis, and hypersegmented neutrophils especially if not corrected with B12 supplementation. Type 2 GNET is associated with MEN-1 syndrome and type 3 is associated with atypical carcinoid syndrome.
Endoscopically type 1 GNETs are most commonly noted in the gastric body or the fundus while type 3 is noted in the antrum. Type 3 is the most aggressive GNET. Endoscopic resection is recommended for type 1 and 2 tumors less than 2 cm. Gastrectomy is required for type 3 GNETs. Endoscopic surveillance every 6-12 months for 3 years and annually thereafter is recommended. Our case highlights the varied role of gastroenterologists in the management of GNETs including diagnosis, staging, treatment, and surveillance.

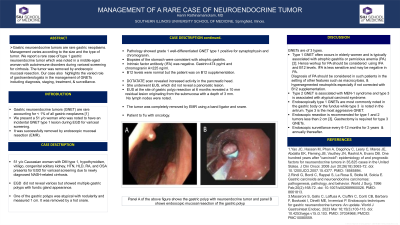
Figure: Panel A of the above figure shows the gastric polyp with neuroendocrine tumor and panel B shows endoscopic mucosal resection of the gastric polyp.
Disclosures:
Harini Rathinamanickam indicated no relevant financial relationships.
Harini Rathinamanickam, MD. P2775 - Management of a Rare Case of Gastric Neuroendocrine Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
