Monday Poster Session
Category: Stomach
P2786 - Delayed Diagnosis of a Gastric Neuroendocrine Tumor: Hindsight Is 20/20
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Umar Siddiqui, DO
University of Texas Health Science Center-San Antonio
Presenting Author(s)
Umar Siddiqui, DO1, Kavea Panneerselvam, MD2, Andrew Han, MD2
1University of Texas Health Science Center-San Antonio, San Antonio, TX; 2University of Texas Health Science Center at San Antonio, San Antonio, TX
Introduction: Gastric neuroendocrine tumors (gNETs) arise from enterochromaffin-like cells in the gastric mucosa. Endoscopically, they can appear as multiple small nodules in the background of atrophic (Type I), hypertrophic mucosa (Type II), or as a single nodule in the background of normal mucosa (Type III). Endoscopically differentiating these lesions from subepithelial lesions (SELs) can be challenging, but prompt and accurate diagnosis of gNETs is crucial to devise a favorable prognosis. Herein we present a case of delayed diagnosis of a gastric NET due to initial endoscopic misdiagnosis.
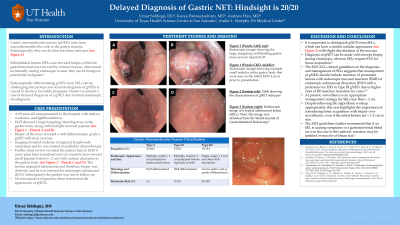
Case Description/Methods: A 69-year-old man presented to the hospital with melena, weakness, and lightheadedness. EGD showed a large, fungating, and bleeding mass in the gastric body, along with multiple mucosal papules (Panels A and B). Biopsy of the mass revealed a well-differentiated, grade 3 gNET with focal necrosis. Further imaging revealed evidence of regional lymph node metastases and he was started on palliative chemotherapy. Further chart review revealed the patient had an EGD 4 years prior (due to melena) and was found to have several small papular lesions with surface ulceration in the gastric body (Panels C and D). The lesions appeared submucosal and therefore, biopsy was deferred, and he was referred for endoscopic ultrasound (EUS). On retrospective inspection, these lesions had the typical appearance of gNETs.
Discussion: gNETs are classified into three subtypes, with Type I being the most common. Type I and Type II gNETs occur in the setting of hypergastrinemia and appear as multiple small yellowish nodules in the gastric body in the background of atrophic or hypertrophic mucosa, respectively. Type III gNETs are sporadic tumors, appear as single lesions, and tend to behave more aggressively than the other two types. It is important to distinguish these lesions from SELs (which can have a similar nodular appearance with slight discoloration of the mucosa), as the diagnostic approach and management of these two entities is different. Diagnosis of gNET can be made with forceps biopsy during endoscopy whereas SELs require EUS for tissue acquisition. The recent ACG clinical guidelines on the diagnosis and management of subepithelial lesions suggests that management of gNETs should include resection of prominent lesions with endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD). A preference for ESD in Type III gNETs is suggested due to higher rates of R0 (complete remission) resection.

Disclosures:
Umar Siddiqui, DO1, Kavea Panneerselvam, MD2, Andrew Han, MD2. P2786 - Delayed Diagnosis of a Gastric Neuroendocrine Tumor: Hindsight Is 20/20, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center-San Antonio, San Antonio, TX; 2University of Texas Health Science Center at San Antonio, San Antonio, TX
Introduction: Gastric neuroendocrine tumors (gNETs) arise from enterochromaffin-like cells in the gastric mucosa. Endoscopically, they can appear as multiple small nodules in the background of atrophic (Type I), hypertrophic mucosa (Type II), or as a single nodule in the background of normal mucosa (Type III). Endoscopically differentiating these lesions from subepithelial lesions (SELs) can be challenging, but prompt and accurate diagnosis of gNETs is crucial to devise a favorable prognosis. Herein we present a case of delayed diagnosis of a gastric NET due to initial endoscopic misdiagnosis.
Case Description/Methods: A 69-year-old man presented to the hospital with melena, weakness, and lightheadedness. EGD showed a large, fungating, and bleeding mass in the gastric body, along with multiple mucosal papules (Panels A and B). Biopsy of the mass revealed a well-differentiated, grade 3 gNET with focal necrosis. Further imaging revealed evidence of regional lymph node metastases and he was started on palliative chemotherapy. Further chart review revealed the patient had an EGD 4 years prior (due to melena) and was found to have several small papular lesions with surface ulceration in the gastric body (Panels C and D). The lesions appeared submucosal and therefore, biopsy was deferred, and he was referred for endoscopic ultrasound (EUS). On retrospective inspection, these lesions had the typical appearance of gNETs.
Discussion: gNETs are classified into three subtypes, with Type I being the most common. Type I and Type II gNETs occur in the setting of hypergastrinemia and appear as multiple small yellowish nodules in the gastric body in the background of atrophic or hypertrophic mucosa, respectively. Type III gNETs are sporadic tumors, appear as single lesions, and tend to behave more aggressively than the other two types. It is important to distinguish these lesions from SELs (which can have a similar nodular appearance with slight discoloration of the mucosa), as the diagnostic approach and management of these two entities is different. Diagnosis of gNET can be made with forceps biopsy during endoscopy whereas SELs require EUS for tissue acquisition. The recent ACG clinical guidelines on the diagnosis and management of subepithelial lesions suggests that management of gNETs should include resection of prominent lesions with endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD). A preference for ESD in Type III gNETs is suggested due to higher rates of R0 (complete remission) resection.

Figure: Panels A and B: Endoscopic images showing the large, fungating, and bleeding gastric mass seen on repeat EGD.
Panels C and D: Endoscopic images showing multiple small nodules in the gastric body that were seen on the initial EGD 4 years prior to presentation.
Panels C and D: Endoscopic images showing multiple small nodules in the gastric body that were seen on the initial EGD 4 years prior to presentation.
Disclosures:
Umar Siddiqui indicated no relevant financial relationships.
Kavea Panneerselvam indicated no relevant financial relationships.
Andrew Han indicated no relevant financial relationships.
Umar Siddiqui, DO1, Kavea Panneerselvam, MD2, Andrew Han, MD2. P2786 - Delayed Diagnosis of a Gastric Neuroendocrine Tumor: Hindsight Is 20/20, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
