Monday Poster Session
Category: Stomach
P2810 - Green Ascites: An Initial Indicator Aiding in the Diagnosis of a Gastric Perforation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Amit Sah, MD
University of Miami at JFK Medical Center
Lantana, FL
Presenting Author(s)
Amit Sah, MD1, Lesley- Ann McCook, MD2, Elizabeth Zakka, MD1, Sumit Sah, BS3, Laura Suzanne Suarez, MD4, Akiva Marcus, MD5
1University of Miami at JFK Medical Center, Lantana, FL; 2University of Miami, Atlantis, FL; 3American University of the Caribbean, Lantana, FL; 4University of Florida Jacksonville, Jacksonville, FL; 5HCA Florida Physicians, JFK Medical Center, West Palm Beach, FL
Introduction: Bilious ascites (BA) or choleperitoneum is caused by post-operative complication of gallbladder or biliary tree perforation, and small bowel perforation. It is confirmed with ascites bilirubin > 6 mg/dL and ascites to serum bilirubin ratio >1. BA as an initial sign of gastric perforation has been rarely reported in literature. Here, we present a case of BA which unmasked a silent gastric perforation.
Case Description/Methods: A 56-years-old male was brought in from prison for generalized weakness and confusion. He was on mycophenolate and prednisone for a recently diagnosed dermatomyositis. Vitals were unremarkable and physical examination on admission was significant for benign abdomen and disorientation to date. Labs significant for WBC 30.8 x 10^3/u, Hgb 10.3 g/dL, AST 157 U/L, ALT 37 U/L, ALP 63 U/L, and total bilirubin 1.6 mg/dL. He was being appropriately treated for MRSA endocarditis.
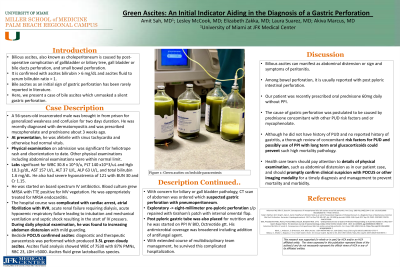
Hospital course was complicated by cardiac arrest, acute renal failure, acute hypoxemic respiratory failure and septic shock. His abdomen was mildly distended and bedside US confirmed ascites. Paracentesis revealed 3.5L green cloudy ascites which grew lactobacillus. Ascites to serum bilirubin ration was 1.5. CT of abdomen suspected gastric perforation with pneumoperitoneum. Exploratory laparotomy revealed a eight-millimeter pre-pyloric perforation. It was repaired with Graham’s patch with internal omental flap. Post pyloric gastric tube was also placed for nutrition and he was started on PPI IV BID, and Octreotide gtt. His antimicrobial coverage was broadened including addition of antifungal agent. With extended course of multidisciplinary team management, he survived this complicated hospitalization.
Discussion: Bilious Ascites can manifest as a sign of peritonitis. Among bowel perforation, BA is usually reported with post-pyloric perforation. Our patient was on high-dose oral prednisone without PPI. The cause of gastric perforation was postulated to be due to prednisone and or mycophenolate. Mycophenolate-related gastrointestinal perforation has also been rarely reported in the literature. A thorough review of concomitant risk factors for PUD and possibly the use of PPI with long-term oral glucocorticoids could prevent such high mortality pathology. The health care team should pay attention to details on physical examination, such as abdominal distension as in our patient's case, and should promptly confirm clinical suspicion with imaging or endoscopy for a timely diagnosis and management.

Disclosures:
Amit Sah, MD1, Lesley- Ann McCook, MD2, Elizabeth Zakka, MD1, Sumit Sah, BS3, Laura Suzanne Suarez, MD4, Akiva Marcus, MD5. P2810 - Green Ascites: An Initial Indicator Aiding in the Diagnosis of a Gastric Perforation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Miami at JFK Medical Center, Lantana, FL; 2University of Miami, Atlantis, FL; 3American University of the Caribbean, Lantana, FL; 4University of Florida Jacksonville, Jacksonville, FL; 5HCA Florida Physicians, JFK Medical Center, West Palm Beach, FL
Introduction: Bilious ascites (BA) or choleperitoneum is caused by post-operative complication of gallbladder or biliary tree perforation, and small bowel perforation. It is confirmed with ascites bilirubin > 6 mg/dL and ascites to serum bilirubin ratio >1. BA as an initial sign of gastric perforation has been rarely reported in literature. Here, we present a case of BA which unmasked a silent gastric perforation.
Case Description/Methods: A 56-years-old male was brought in from prison for generalized weakness and confusion. He was on mycophenolate and prednisone for a recently diagnosed dermatomyositis. Vitals were unremarkable and physical examination on admission was significant for benign abdomen and disorientation to date. Labs significant for WBC 30.8 x 10^3/u, Hgb 10.3 g/dL, AST 157 U/L, ALT 37 U/L, ALP 63 U/L, and total bilirubin 1.6 mg/dL. He was being appropriately treated for MRSA endocarditis.
Hospital course was complicated by cardiac arrest, acute renal failure, acute hypoxemic respiratory failure and septic shock. His abdomen was mildly distended and bedside US confirmed ascites. Paracentesis revealed 3.5L green cloudy ascites which grew lactobacillus. Ascites to serum bilirubin ration was 1.5. CT of abdomen suspected gastric perforation with pneumoperitoneum. Exploratory laparotomy revealed a eight-millimeter pre-pyloric perforation. It was repaired with Graham’s patch with internal omental flap. Post pyloric gastric tube was also placed for nutrition and he was started on PPI IV BID, and Octreotide gtt. His antimicrobial coverage was broadened including addition of antifungal agent. With extended course of multidisciplinary team management, he survived this complicated hospitalization.
Discussion: Bilious Ascites can manifest as a sign of peritonitis. Among bowel perforation, BA is usually reported with post-pyloric perforation. Our patient was on high-dose oral prednisone without PPI. The cause of gastric perforation was postulated to be due to prednisone and or mycophenolate. Mycophenolate-related gastrointestinal perforation has also been rarely reported in the literature. A thorough review of concomitant risk factors for PUD and possibly the use of PPI with long-term oral glucocorticoids could prevent such high mortality pathology. The health care team should pay attention to details on physical examination, such as abdominal distension as in our patient's case, and should promptly confirm clinical suspicion with imaging or endoscopy for a timely diagnosis and management.

Figure: Bilious ascites during paracentesis.
Disclosures:
Amit Sah indicated no relevant financial relationships.
Lesley- Ann McCook indicated no relevant financial relationships.
Elizabeth Zakka indicated no relevant financial relationships.
Sumit Sah indicated no relevant financial relationships.
Laura Suzanne Suarez indicated no relevant financial relationships.
Akiva Marcus indicated no relevant financial relationships.
Amit Sah, MD1, Lesley- Ann McCook, MD2, Elizabeth Zakka, MD1, Sumit Sah, BS3, Laura Suzanne Suarez, MD4, Akiva Marcus, MD5. P2810 - Green Ascites: An Initial Indicator Aiding in the Diagnosis of a Gastric Perforation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
