Monday Poster Session
Category: Stomach
P2814 - Endoscopic Evaluation Leading to Diagnosis of Hereditary Angioedema
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Scarlett Austin, DO
Allegheny Health Network
Pittsburgh, PA
Presenting Author(s)
Scarlett Austin, DO1, Evan H. Reinhart, DO2, Mohamed Eisa, MD1
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: We describe a case of severe abdominal pain following an uneventful upper endoscopy, which led to a diagnosis of Hereditary Angioedema (HAE). Given symptoms, recent procedure, and pertinent family history, testing was pursued and diagnostic of HAE.
Case Description/Methods: Patient is a 27-year-old female with history of asthma, who presented to an outpatient Gastroenterology appointment due to nausea, bloating, and intermittent abdominal pain. Celiac disease and gastroparesis were ruled out. Patient had an upper endoscopy with normal esophagus, stomach, and duodenum. Biopsies were taken to evaluate for helicobacter pylori infection and celiac disease.
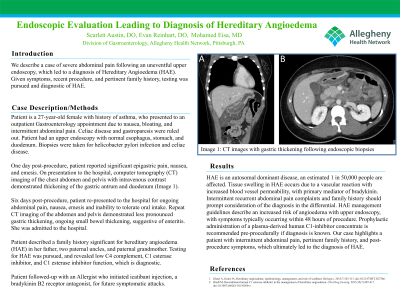
One day post-procedure, patient reported significant epigastric pain, nausea, and emesis. On presentation to the hospital, computed tomography (CT) imaging of the chest, abdomen and pelvis with intravenous contrast demonstrated thickening of gastric antrum and duodenum.
Six days post-procedure, patient re-presented to the hospital for ongoing abdominal pain, nausea, emesis and inability to tolerate oral intake. Repeat CT imaging of abdomen and pelvis demonstrated less pronounced gastric thickening, ongoing small bowel thickening, suggestive of enteritis. She was admitted to the hospital.
Patient described a family history significant for hereditary angioedema (HAE) in her father, two paternal uncles, and paternal grandmother. Testing for HAE was pursued, and revealed low C4 complement, C1 esterase inhibitor, and C1 esterase inhibitor function, which is diagnostic.
Patient followed-up with an Allergist who initiated icatibant injection, a bradykinin B2 receptor antagonist, for future symptomatic attacks.
Discussion: HAE is an autosomal dominant disease, an estimated 1 in 50,000 people are affected. Tissue swelling in HAE occurs due to a vascular reaction with increased blood vessel permeability, with primary mediator of bradykinin. Intermittent recurrent abdominal pain complaints and family history should prompt consideration of the diagnosis in the differential. HAE management guidelines describe increased risk of angioedema with upper endoscopy, with symptoms typically occurring within 48 hours of procedure. Prophylactic administration of a plasma-derived human C1-inhibitor concentrate is recommended pre-procedurally if diagnosis is known. Our case highlights a patient with intermittent abdominal pain, pertinent family history, and post-procedure symptoms, which ultimately led to the diagnosis of HAE.

Disclosures:
Scarlett Austin, DO1, Evan H. Reinhart, DO2, Mohamed Eisa, MD1. P2814 - Endoscopic Evaluation Leading to Diagnosis of Hereditary Angioedema, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Allegheny Health Network, Pittsburgh, PA; 2Allegheny General Hospital, Pittsburgh, PA
Introduction: We describe a case of severe abdominal pain following an uneventful upper endoscopy, which led to a diagnosis of Hereditary Angioedema (HAE). Given symptoms, recent procedure, and pertinent family history, testing was pursued and diagnostic of HAE.
Case Description/Methods: Patient is a 27-year-old female with history of asthma, who presented to an outpatient Gastroenterology appointment due to nausea, bloating, and intermittent abdominal pain. Celiac disease and gastroparesis were ruled out. Patient had an upper endoscopy with normal esophagus, stomach, and duodenum. Biopsies were taken to evaluate for helicobacter pylori infection and celiac disease.
One day post-procedure, patient reported significant epigastric pain, nausea, and emesis. On presentation to the hospital, computed tomography (CT) imaging of the chest, abdomen and pelvis with intravenous contrast demonstrated thickening of gastric antrum and duodenum.
Six days post-procedure, patient re-presented to the hospital for ongoing abdominal pain, nausea, emesis and inability to tolerate oral intake. Repeat CT imaging of abdomen and pelvis demonstrated less pronounced gastric thickening, ongoing small bowel thickening, suggestive of enteritis. She was admitted to the hospital.
Patient described a family history significant for hereditary angioedema (HAE) in her father, two paternal uncles, and paternal grandmother. Testing for HAE was pursued, and revealed low C4 complement, C1 esterase inhibitor, and C1 esterase inhibitor function, which is diagnostic.
Patient followed-up with an Allergist who initiated icatibant injection, a bradykinin B2 receptor antagonist, for future symptomatic attacks.
Discussion: HAE is an autosomal dominant disease, an estimated 1 in 50,000 people are affected. Tissue swelling in HAE occurs due to a vascular reaction with increased blood vessel permeability, with primary mediator of bradykinin. Intermittent recurrent abdominal pain complaints and family history should prompt consideration of the diagnosis in the differential. HAE management guidelines describe increased risk of angioedema with upper endoscopy, with symptoms typically occurring within 48 hours of procedure. Prophylactic administration of a plasma-derived human C1-inhibitor concentrate is recommended pre-procedurally if diagnosis is known. Our case highlights a patient with intermittent abdominal pain, pertinent family history, and post-procedure symptoms, which ultimately led to the diagnosis of HAE.

Figure: CT images with gastric thickening following endoscopic biopsies
Disclosures:
Scarlett Austin indicated no relevant financial relationships.
Evan Reinhart indicated no relevant financial relationships.
Mohamed Eisa indicated no relevant financial relationships.
Scarlett Austin, DO1, Evan H. Reinhart, DO2, Mohamed Eisa, MD1. P2814 - Endoscopic Evaluation Leading to Diagnosis of Hereditary Angioedema, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
