Monday Poster Session
Category: Stomach
P2823 - Gastrointestinal Amyloidosis – An Unusual Cause Iron Deficiency Anemia
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Justice Arhinful, MD
Howard University Hospital
Washington, DC
Presenting Author(s)
Justice Arhinful, MD, Suryanarayana Reddy Challa, MD, Philip Oppong-Twene, MD, MPH, Devon Jackson, MD, Babak Shokrani, MD, Laiyemo Adeyinka, MD, MPH, FACG
Howard University Hospital, Washington, DC
Introduction: Amyloidosis is a rare heterogenous group of disorders characterized by the extracellular deposition of autologous, insoluble, fibrillar misfolded proteins in various tissues. GI manifestations include malabsorption, diarrhea, GI bleed, and protein-losing enteropathy. Iron deficiency as the initial manifestation GI amyloidosis without any overt GI symptoms is rare. We present a case of amyloidosis involving the stomach and duodenum presenting as severe symptomatic iron deficiency anemia.
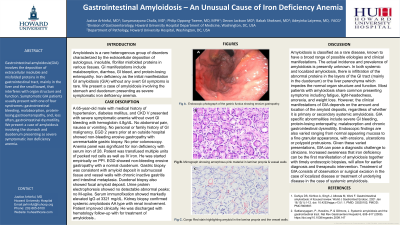
Case Description/Methods: A 65-year-old male with past medical history of hypertension, diabetes mellitus, and CKD stage V presented with severe symptomatic anemia without overt GI bleeding. GI was consulted on account of anemia (with Hgb 4.8g/dL) with positive FOBT. No abdominal pain, nausea or vomiting. No personal or family history of GI malignancy. EGD 2 years prior at an outside hospital showed non-bleeding erosive gastropathy. No prior colonoscopy. Anemia panel was significant for iron deficiency with serum iron of 28. Patient was transfused multiple units of packed red cells as well as IV iron. He was started empirically on PPI. EGD showed non-bleeding erosive gastropathy with a normal duodenum. Gastric biopsy was consistent with amyloid deposit in submucosal tissue and vessel walls with chronic inactive gastritis and intestinal metaplasia. Duodenal biopsy also showed focal amyloid deposit. Urine protein electrophoresis showed no detectable abnormal peaks; no M-spike. Serum immunofixation showed markedly elevated IgG at 3321 mg/dL. Patient improved clinically. He was discharged with hematology follow-up with the plan to do additional work up for amyloidosis.
Discussion: GI amyloidosis involves the extracellular deposition of insoluble misfolded proteins, mainly in the duodenum which impedes the normal organ structure and function. Clinical manifestations of GIA are varied and range from nausea to severe GI bleeding. Endoscopic findings are also varied ranging from normal appearing mucosa to a fine granular appearance, with erosions, ulcerations or polypoid protrusions. Given these varied presentations, GIA can pose a diagnostic challenge to clinicians. Increased awareness that iron deficiency can be the first manifestation of amyloidosis together with timely endoscopic biopsies, will allow for earlier diagnosis and therapeutic intervention. Treatment of GIA consists of observation or surgical excision in the case of localized disease or treatment of underlying disease in the case of systemic amyloidosis.

Disclosures:
Justice Arhinful, MD, Suryanarayana Reddy Challa, MD, Philip Oppong-Twene, MD, MPH, Devon Jackson, MD, Babak Shokrani, MD, Laiyemo Adeyinka, MD, MPH, FACG. P2823 - Gastrointestinal Amyloidosis – An Unusual Cause Iron Deficiency Anemia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Howard University Hospital, Washington, DC
Introduction: Amyloidosis is a rare heterogenous group of disorders characterized by the extracellular deposition of autologous, insoluble, fibrillar misfolded proteins in various tissues. GI manifestations include malabsorption, diarrhea, GI bleed, and protein-losing enteropathy. Iron deficiency as the initial manifestation GI amyloidosis without any overt GI symptoms is rare. We present a case of amyloidosis involving the stomach and duodenum presenting as severe symptomatic iron deficiency anemia.
Case Description/Methods: A 65-year-old male with past medical history of hypertension, diabetes mellitus, and CKD stage V presented with severe symptomatic anemia without overt GI bleeding. GI was consulted on account of anemia (with Hgb 4.8g/dL) with positive FOBT. No abdominal pain, nausea or vomiting. No personal or family history of GI malignancy. EGD 2 years prior at an outside hospital showed non-bleeding erosive gastropathy. No prior colonoscopy. Anemia panel was significant for iron deficiency with serum iron of 28. Patient was transfused multiple units of packed red cells as well as IV iron. He was started empirically on PPI. EGD showed non-bleeding erosive gastropathy with a normal duodenum. Gastric biopsy was consistent with amyloid deposit in submucosal tissue and vessel walls with chronic inactive gastritis and intestinal metaplasia. Duodenal biopsy also showed focal amyloid deposit. Urine protein electrophoresis showed no detectable abnormal peaks; no M-spike. Serum immunofixation showed markedly elevated IgG at 3321 mg/dL. Patient improved clinically. He was discharged with hematology follow-up with the plan to do additional work up for amyloidosis.
Discussion: GI amyloidosis involves the extracellular deposition of insoluble misfolded proteins, mainly in the duodenum which impedes the normal organ structure and function. Clinical manifestations of GIA are varied and range from nausea to severe GI bleeding. Endoscopic findings are also varied ranging from normal appearing mucosa to a fine granular appearance, with erosions, ulcerations or polypoid protrusions. Given these varied presentations, GIA can pose a diagnostic challenge to clinicians. Increased awareness that iron deficiency can be the first manifestation of amyloidosis together with timely endoscopic biopsies, will allow for earlier diagnosis and therapeutic intervention. Treatment of GIA consists of observation or surgical excision in the case of localized disease or treatment of underlying disease in the case of systemic amyloidosis.

Figure: A: Gastric fundus showing erosive gastropathy
B: High magnification showing amorphous pink material in laminar propria and vessel walls
C: High magnification with Congo Red stain highlighting amyloid in the lamina propria and the vessel walls
B: High magnification showing amorphous pink material in laminar propria and vessel walls
C: High magnification with Congo Red stain highlighting amyloid in the lamina propria and the vessel walls
Disclosures:
Justice Arhinful indicated no relevant financial relationships.
Suryanarayana Reddy Challa indicated no relevant financial relationships.
Philip Oppong-Twene indicated no relevant financial relationships.
Devon Jackson indicated no relevant financial relationships.
Babak Shokrani indicated no relevant financial relationships.
Laiyemo Adeyinka indicated no relevant financial relationships.
Justice Arhinful, MD, Suryanarayana Reddy Challa, MD, Philip Oppong-Twene, MD, MPH, Devon Jackson, MD, Babak Shokrani, MD, Laiyemo Adeyinka, MD, MPH, FACG. P2823 - Gastrointestinal Amyloidosis – An Unusual Cause Iron Deficiency Anemia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
