Monday Poster Session
Category: Stomach
P2825 - Gastric Linitis vs Gastric Wall Thickening - A Case Series
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- BG
Brandon Gordon, MD
Internal Medicine
Fort Wayne, IN
Presenting Author(s)
Brandon Gordon, MD
Internal Medicine, Fort Wayne, IN
Introduction: Gastric wall thickening can be characterized by inelastic portion of the stomach. Initial diagnostic upper EGDs with biopsies may fail to demonstrate the classic histopathological changes. Recommended workup algorithms recommend EUS-FNA as an effective modality due to the possibility of false negative. We will discuss how EUS-FNA assisted in making the diagnosis.
Case Description/Methods: Case 1 presented initially to her PCP with abdominal pain and weight loss. Her symptoms were attributed to a positive H. Pylori test to which she was treated. Her symptoms persisted. Upper EGD was performed and demonstrated diffuse edema erythema and friability most concerning for severe gastritis. Initial biopsy results were negative and the patient’s working diagnosis was atrophic chronic gastritis. In repeat EGD, diffuse gastric atrophy and thick gastric mucosa involving the entire stomach was noted and multiple biopsies obtained. The patient symptoms continued to persist. CTAP demonstrated diffuse thickening of the gastric wall and early linitis plastica was suspected. She was started on omeprazole daily. Symptoms largely resolved aside from intermittent lower abdominal pain. Subsequent EGD resulted in spontaneous bleeding from the gastric mucosa and Prilosec + triple therapy initiated. The patient continued to have symptoms & EGD+EUS with bite on bite biopsies scheduled. Finally, results revealed signet cells involving the submucosal layers of the stomach. Remarkably, the patients symptoms largely resolved on BID PPI.
Case 2 is a 63 year old male who originally presented with nausea, vomiting and severe abdominal pain. He was hospitalized after a MRE demonstrated proximal gastric wall thickening & mucosal hyper enhancement enhancement. EGD/EUS demonstrated findings consistent with erosive esophagitis and an abnormally thickened mucosa in the proximal half of the stomach. However, biopsies were obtained and did not demonstrate histopathlogical abnormalities. Treatment was initiated with daily PPI and Bentyl. His symptoms gradually resolved.
Discussion: Symptoms of LP can be attributed to increased rigidity of the stomach and interruption of peristalsis. Malignant cells are frequently quite deep beyond the mucosa. Multiple biopsies including EUS may be necessary. Treatment can include radiotherapy, chemotherapy as well as radical surgery. In the series above, both patients demonstrated abnormal wall thickening without classic findings on biopsy and are responding well to management including PPIs and Bentyl.

Disclosures:
Brandon Gordon, MD. P2825 - Gastric Linitis vs Gastric Wall Thickening - A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Internal Medicine, Fort Wayne, IN
Introduction: Gastric wall thickening can be characterized by inelastic portion of the stomach. Initial diagnostic upper EGDs with biopsies may fail to demonstrate the classic histopathological changes. Recommended workup algorithms recommend EUS-FNA as an effective modality due to the possibility of false negative. We will discuss how EUS-FNA assisted in making the diagnosis.
Case Description/Methods: Case 1 presented initially to her PCP with abdominal pain and weight loss. Her symptoms were attributed to a positive H. Pylori test to which she was treated. Her symptoms persisted. Upper EGD was performed and demonstrated diffuse edema erythema and friability most concerning for severe gastritis. Initial biopsy results were negative and the patient’s working diagnosis was atrophic chronic gastritis. In repeat EGD, diffuse gastric atrophy and thick gastric mucosa involving the entire stomach was noted and multiple biopsies obtained. The patient symptoms continued to persist. CTAP demonstrated diffuse thickening of the gastric wall and early linitis plastica was suspected. She was started on omeprazole daily. Symptoms largely resolved aside from intermittent lower abdominal pain. Subsequent EGD resulted in spontaneous bleeding from the gastric mucosa and Prilosec + triple therapy initiated. The patient continued to have symptoms & EGD+EUS with bite on bite biopsies scheduled. Finally, results revealed signet cells involving the submucosal layers of the stomach. Remarkably, the patients symptoms largely resolved on BID PPI.
Case 2 is a 63 year old male who originally presented with nausea, vomiting and severe abdominal pain. He was hospitalized after a MRE demonstrated proximal gastric wall thickening & mucosal hyper enhancement enhancement. EGD/EUS demonstrated findings consistent with erosive esophagitis and an abnormally thickened mucosa in the proximal half of the stomach. However, biopsies were obtained and did not demonstrate histopathlogical abnormalities. Treatment was initiated with daily PPI and Bentyl. His symptoms gradually resolved.
Discussion: Symptoms of LP can be attributed to increased rigidity of the stomach and interruption of peristalsis. Malignant cells are frequently quite deep beyond the mucosa. Multiple biopsies including EUS may be necessary. Treatment can include radiotherapy, chemotherapy as well as radical surgery. In the series above, both patients demonstrated abnormal wall thickening without classic findings on biopsy and are responding well to management including PPIs and Bentyl.

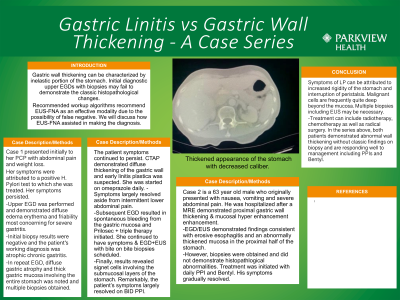
Figure: Thickened appearance of the stomach with decreased caliber.
Disclosures:
Brandon Gordon indicated no relevant financial relationships.
Brandon Gordon, MD. P2825 - Gastric Linitis vs Gastric Wall Thickening - A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
