Monday Poster Session
Category: Stomach
P2756 - Beneath the Surface: A Comprehensive Exploration of Gastrointestinal Motility Disorders Post Kidney Transplantation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpeg.jpg)
Xiaoliang Wang, MD, PhD
Marshall University School of Medicine
Huntington, WV
Presenting Author(s)
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: In the realm of kidney transplant (KT) recipient care, the link to gastrointestinal (GI) motility disorders, such as gastroesophageal reflux disease (GERD), gastroparesis, and irritable bowel syndrome (IBS), remains elusive and intriguing. These disorders present a symptom constellation impacting patient quality of life, yet remain poorly understood. Our large-scale, population-based study endeavors to untangle this intricate relationship.
Methods: In this study, we analyzed the Population-based National Inpatient Sample data, which encompassed 7,159,694 patients. Our inclusion criteria comprised patients diagnosed with gastroparesis (ICD-10 K31.84), GERD (ICD-10 K21), and IBS (ICD-10 K58), with or without a history of KT (ICD-10 Z94.0), excluding those with other organ transplants. We adjusted for various risk factors including age, gender, race, type 2 diabetes mellitus (T2DM), smoking, hiatal hernia, and obesity. Our analytical focus was on the prevalence and odds ratios of these GI motility disorders in the KT cohort, and the co-existence of these disorders, assessed through stringent statistical evaluations.
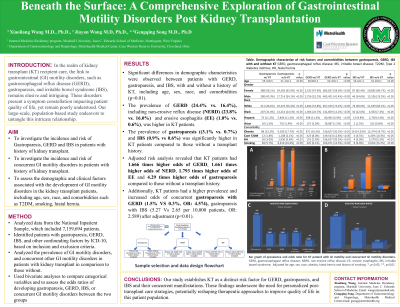
Results: Significant demographic differences were observed between GERD, gastroparesis, and IBS patients, with and without a history of KT, including age, sex, race, and comorbidities (p< 0.01). Interestingly, KT patients had a higher prevalence of GERD (24.4% vs. 16.4%, p< 0.01), including NERD (23.8% vs. 16.0%, p< 0.01) and erosive esophagitis (1.0% vs. 0.6%, p< 0.01). KT patients also had a significantly higher prevalence of gastroparesis (3.1% vs. 0.7%, p< 0.01) and IBS (0.9% vs. 0.6%). Adjusted risk analysis revealed that KT patients had 1.666 times higher odds of GERD, 1.661 times higher odds of NERD, 1.793 times higher odds of erosive esophagitis, and 4.29 times higher odds of gastroparesis compared to those without a transplant history. Additionally, KT patients had a higher prevalence and increased odds of concurrent gastroparesis with GERD (1.5% vs. 0.3%, OR: 4.574) and gastroparesis with IBS (5.27 vs. 2.65 per 10,000 patients, OR: 2.589) after adjustment (p< 0.01). No significant association was found between KT and patients with concurrent GERD and IBS.
Discussion: Our study establishes KT as a distinct risk factor for GERD, gastroparesis, and IBS and their concurrent manifestations. These findings underscore the need for personalized post-transplant care strategies, potentially reshaping therapeutic approaches to improve quality of life in this patient population.

Disclosures:
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2. P2756 - Beneath the Surface: A Comprehensive Exploration of Gastrointestinal Motility Disorders Post Kidney Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: In the realm of kidney transplant (KT) recipient care, the link to gastrointestinal (GI) motility disorders, such as gastroesophageal reflux disease (GERD), gastroparesis, and irritable bowel syndrome (IBS), remains elusive and intriguing. These disorders present a symptom constellation impacting patient quality of life, yet remain poorly understood. Our large-scale, population-based study endeavors to untangle this intricate relationship.
Methods: In this study, we analyzed the Population-based National Inpatient Sample data, which encompassed 7,159,694 patients. Our inclusion criteria comprised patients diagnosed with gastroparesis (ICD-10 K31.84), GERD (ICD-10 K21), and IBS (ICD-10 K58), with or without a history of KT (ICD-10 Z94.0), excluding those with other organ transplants. We adjusted for various risk factors including age, gender, race, type 2 diabetes mellitus (T2DM), smoking, hiatal hernia, and obesity. Our analytical focus was on the prevalence and odds ratios of these GI motility disorders in the KT cohort, and the co-existence of these disorders, assessed through stringent statistical evaluations.
Results: Significant demographic differences were observed between GERD, gastroparesis, and IBS patients, with and without a history of KT, including age, sex, race, and comorbidities (p< 0.01). Interestingly, KT patients had a higher prevalence of GERD (24.4% vs. 16.4%, p< 0.01), including NERD (23.8% vs. 16.0%, p< 0.01) and erosive esophagitis (1.0% vs. 0.6%, p< 0.01). KT patients also had a significantly higher prevalence of gastroparesis (3.1% vs. 0.7%, p< 0.01) and IBS (0.9% vs. 0.6%). Adjusted risk analysis revealed that KT patients had 1.666 times higher odds of GERD, 1.661 times higher odds of NERD, 1.793 times higher odds of erosive esophagitis, and 4.29 times higher odds of gastroparesis compared to those without a transplant history. Additionally, KT patients had a higher prevalence and increased odds of concurrent gastroparesis with GERD (1.5% vs. 0.3%, OR: 4.574) and gastroparesis with IBS (5.27 vs. 2.65 per 10,000 patients, OR: 2.589) after adjustment (p< 0.01). No significant association was found between KT and patients with concurrent GERD and IBS.
Discussion: Our study establishes KT as a distinct risk factor for GERD, gastroparesis, and IBS and their concurrent manifestations. These findings underscore the need for personalized post-transplant care strategies, potentially reshaping therapeutic approaches to improve quality of life in this patient population.

Figure: Figure A, Demographic characterize, risk factors and comorbidities between Kidney transplants with and without gastroparesis, GERD, or IBS. B, Prevalence and odds ratio of gastroparesis, GERD, IBS, and concurrent GI motility diseases in patients with history of kidney transplant. C, Bar graph of prevalence and odds ratio of gastroparesis, GERD, IBS, and concurrent GI motility diseases in patients with history of kidney transplant. GERD, gastroesophageal reflux disease; NERD, non-erosive reflex disease; IBS, irritable bowel syndrome, KT, kidney transplantation *, p<0.05; **, p<0.01
Disclosures:
Xiaoliang Wang indicated no relevant financial relationships.
Jiayan Wang indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2. P2756 - Beneath the Surface: A Comprehensive Exploration of Gastrointestinal Motility Disorders Post Kidney Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
