Monday Poster Session
Category: Interventional Endoscopy
P2314 - Endoscopic Management of Bouveret Syndrome After Complex Thoracic and Foregut Surgery
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Shyamal Sheth, DO
Franciscan Health Olympia Fields
Olympia Fields, IL
Presenting Author(s)
Shyamal Sheth, DO1, Agnieska Maniak, MD2, Nicole Geissen, MD2, Neal Mehta, MD2
1Franciscan Health Olympia Fields, Chicago, IL; 2Rush University Medical Center, Chicago, IL
Introduction: Bouveret syndrome is a rare complication of gallstone ileus, characterized by gastric outlet obstruction at the pylorus or proximal duodenum due to the presence of a large gallstone. Herein, we present a case of Bouveret syndrome after a complex surgical intervention associated with a cholecystogastric fistula, which was successfully managed through endoscopic stone extraction.
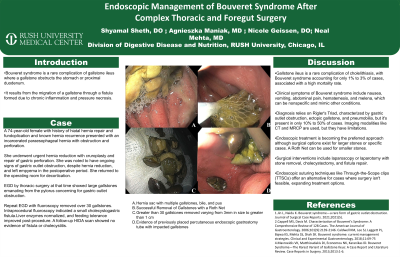
Case Description/Methods: A 74-year-old female with a history of hiatal hernia s/p Nissen fundoplication presented as a transfer for a perforated incarcerated paraesophageal hernia and a large loculated pleural effusion. She underwent a reduction of the paraesophageal hernia with cruroplasty and gastric wedge resection. Subsequently, she continued to have a large pleural effusion, inability to tolerate post-pyloric feeding, and rising liver enzymes concerning for acalculous cholecystitis. In the OR, the patient underwent thoracotomy for the effusion and esophagogastroduodenoscopy (EGD) initially with thoracic surgery that showed numerous large gallstones in the pylorus, causing downstream obstruction. Given concern for cholecystoduodenal fistula, interventional gastroenterology was consulted. MRCP did not demonstrate any signs of a cholecystoduodenal fistula, such as the presence of gas within the gallbladder lumen, pneumobilia, or dilated ducts. Given the OR EGD findings, repeat EGD with fluoroscopy was performed, which revealed more than 30 gallstones within the hernia sac, a collection of pus and bile, as well as multiple gallstones at the gastric pylorus (Figure 1). All the gallstones were successfully extracted using an overtube and a retrieval net. Intraprocedural fluoroscopy indicated the presence of a small cholecystogastric fistula involving the herniated sac. The tract appeared to be healing and the opening was small. Following the EGD, the patient's liver enzymes slowly normalized and she was able to tolerate post-pyloric tube feeding. Ten days later, a hepatobiliary iminodiacetic acid (HIDA) scan showed no evidence of biliary extravasation or fistula, patent common bile duct and cystic duct, and no signs of acalculous cholecystitis.
Discussion: The hallmark signs of Bouveret syndrome, known as Rigler's Triad, consist of gastric outlet obstruction, ectopic gallstones, and pneumobilia. However, all three components of Rigler's Triad are not always present. Optimal treatment for Bouveret syndrome remains controversial, however endoscopic treatment is a feasible option, especially in high-risk patients.

Disclosures:
Shyamal Sheth, DO1, Agnieska Maniak, MD2, Nicole Geissen, MD2, Neal Mehta, MD2. P2314 - Endoscopic Management of Bouveret Syndrome After Complex Thoracic and Foregut Surgery, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Franciscan Health Olympia Fields, Chicago, IL; 2Rush University Medical Center, Chicago, IL
Introduction: Bouveret syndrome is a rare complication of gallstone ileus, characterized by gastric outlet obstruction at the pylorus or proximal duodenum due to the presence of a large gallstone. Herein, we present a case of Bouveret syndrome after a complex surgical intervention associated with a cholecystogastric fistula, which was successfully managed through endoscopic stone extraction.
Case Description/Methods: A 74-year-old female with a history of hiatal hernia s/p Nissen fundoplication presented as a transfer for a perforated incarcerated paraesophageal hernia and a large loculated pleural effusion. She underwent a reduction of the paraesophageal hernia with cruroplasty and gastric wedge resection. Subsequently, she continued to have a large pleural effusion, inability to tolerate post-pyloric feeding, and rising liver enzymes concerning for acalculous cholecystitis. In the OR, the patient underwent thoracotomy for the effusion and esophagogastroduodenoscopy (EGD) initially with thoracic surgery that showed numerous large gallstones in the pylorus, causing downstream obstruction. Given concern for cholecystoduodenal fistula, interventional gastroenterology was consulted. MRCP did not demonstrate any signs of a cholecystoduodenal fistula, such as the presence of gas within the gallbladder lumen, pneumobilia, or dilated ducts. Given the OR EGD findings, repeat EGD with fluoroscopy was performed, which revealed more than 30 gallstones within the hernia sac, a collection of pus and bile, as well as multiple gallstones at the gastric pylorus (Figure 1). All the gallstones were successfully extracted using an overtube and a retrieval net. Intraprocedural fluoroscopy indicated the presence of a small cholecystogastric fistula involving the herniated sac. The tract appeared to be healing and the opening was small. Following the EGD, the patient's liver enzymes slowly normalized and she was able to tolerate post-pyloric tube feeding. Ten days later, a hepatobiliary iminodiacetic acid (HIDA) scan showed no evidence of biliary extravasation or fistula, patent common bile duct and cystic duct, and no signs of acalculous cholecystitis.
Discussion: The hallmark signs of Bouveret syndrome, known as Rigler's Triad, consist of gastric outlet obstruction, ectopic gallstones, and pneumobilia. However, all three components of Rigler's Triad are not always present. Optimal treatment for Bouveret syndrome remains controversial, however endoscopic treatment is a feasible option, especially in high-risk patients.

Figure: A.Hernia sac with multiple gallstones, bile and pus
B. Successful removal of gallstones with Roth net
C. Greater than 30 gallstones removed varying from 3 mm in size to greater than 1 cm
D. Evidence of previously placed percutaneous endoscopic gastrostomy tube with impacted gallstones
B. Successful removal of gallstones with Roth net
C. Greater than 30 gallstones removed varying from 3 mm in size to greater than 1 cm
D. Evidence of previously placed percutaneous endoscopic gastrostomy tube with impacted gallstones
Disclosures:
Shyamal Sheth indicated no relevant financial relationships.
Agnieska Maniak indicated no relevant financial relationships.
Nicole Geissen indicated no relevant financial relationships.
Neal Mehta indicated no relevant financial relationships.
Shyamal Sheth, DO1, Agnieska Maniak, MD2, Nicole Geissen, MD2, Neal Mehta, MD2. P2314 - Endoscopic Management of Bouveret Syndrome After Complex Thoracic and Foregut Surgery, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
