Monday Poster Session
Category: GI Bleeding
P2108 - Gastric Amyloidosis: A Rare Cause of Hematemesis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Neel Matiwala, BS
Saint Louis University
St. Louis, MO
Presenting Author(s)
Neel Matiwala, BS, Rohan Tripathi, BS, Hayden Rotramel, MD, Ameya deshmukh, DO, Jay Shah, DO, Abdallah El Alayli, MD, Maya Mahmoud, MD, Eyad Gharaibeh, MD, Jennifer Palagiri, MD
Saint Louis University, St. Louis, MO
Introduction: Amyloid light chain (AL) amyloidosis is caused by the uncontrolled production of light chains by plasma cell dyscrasias. Although any organ is susceptible to light chain deposition, classically, deposition occurs in the heart, liver or kidneys presenting with symptoms of restrictive cardiomyopathy, hepatomegaly or nephrotic syndrome. We present a case of amyloid deposition in the gastric body causing hematemesis.
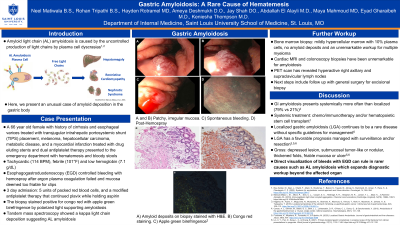
Case Description/Methods: A 66-year-old female with history of cirrhosis and esophageal varices treated with transjugular intrahepatic portosystemic shunt placement presented to the emergency department with hematemesis and bloody stools. She was tachycardic (114 BPM), febrile (101°F) and anemic (7.1 g/dL). Esophagogastroduodenoscopy (EGD) revealed a patchy, mucosal abnormality in the body of the stomach bleeding spontaneously from multiple sites that worsened with contact, suctioning, and water jet. The bleeding was controlled by hemospray after argon plasma coagulation failed. The gastric mucosa was too thin and friable for clip placement. Biopsies of adjacent mucosa was obtained for histology. Throughout the 3-day admission, the patient was given 5 units of packed red blood cells, and a modified antiplatelet therapy that continued plavix while holding aspirin. The biopsy stained positive for congo red with apple green birefringence by polarized light supporting amyloidosis. Mass spectroscopy showed a kappa light chain deposition suggesting AL amyloidosis. Follow up with hematology and bone marrow biopsy revealed a mildly hypercellular marrow with 10% plasma cells, no amyloid deposits and an unremarkable workup for multiple myeloma. Cardiac MRI and colonoscopy biopsies have been negative for amyloidosis. PET scan has revealed hyperactive right axillary and supraclavicular lymph nodes. Next steps include follow up with general surgery for excisional biopsy to differentiate between localized or systemic amyloidosis, or another malignancy.
Discussion: Hematemesis and hematochezia in patients with cirrhosis would be unlikely to raise suspicion for amyloidosis. Endoscopic visualization of gastric mucosa can capture rarer etiologies of GI bleeding such as AL amyloidosis which expands workup beyond the affected organ. GI amyloidosis presents systemically more often than localized. While systemic disease is managed with chemo/immunotherapy and/or hematopoietic cell transplant, localized GI amyloidosis continues to be a rare disease without specific guidelines for management.

Disclosures:
Neel Matiwala, BS, Rohan Tripathi, BS, Hayden Rotramel, MD, Ameya deshmukh, DO, Jay Shah, DO, Abdallah El Alayli, MD, Maya Mahmoud, MD, Eyad Gharaibeh, MD, Jennifer Palagiri, MD. P2108 - Gastric Amyloidosis: A Rare Cause of Hematemesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Saint Louis University, St. Louis, MO
Introduction: Amyloid light chain (AL) amyloidosis is caused by the uncontrolled production of light chains by plasma cell dyscrasias. Although any organ is susceptible to light chain deposition, classically, deposition occurs in the heart, liver or kidneys presenting with symptoms of restrictive cardiomyopathy, hepatomegaly or nephrotic syndrome. We present a case of amyloid deposition in the gastric body causing hematemesis.
Case Description/Methods: A 66-year-old female with history of cirrhosis and esophageal varices treated with transjugular intrahepatic portosystemic shunt placement presented to the emergency department with hematemesis and bloody stools. She was tachycardic (114 BPM), febrile (101°F) and anemic (7.1 g/dL). Esophagogastroduodenoscopy (EGD) revealed a patchy, mucosal abnormality in the body of the stomach bleeding spontaneously from multiple sites that worsened with contact, suctioning, and water jet. The bleeding was controlled by hemospray after argon plasma coagulation failed. The gastric mucosa was too thin and friable for clip placement. Biopsies of adjacent mucosa was obtained for histology. Throughout the 3-day admission, the patient was given 5 units of packed red blood cells, and a modified antiplatelet therapy that continued plavix while holding aspirin. The biopsy stained positive for congo red with apple green birefringence by polarized light supporting amyloidosis. Mass spectroscopy showed a kappa light chain deposition suggesting AL amyloidosis. Follow up with hematology and bone marrow biopsy revealed a mildly hypercellular marrow with 10% plasma cells, no amyloid deposits and an unremarkable workup for multiple myeloma. Cardiac MRI and colonoscopy biopsies have been negative for amyloidosis. PET scan has revealed hyperactive right axillary and supraclavicular lymph nodes. Next steps include follow up with general surgery for excisional biopsy to differentiate between localized or systemic amyloidosis, or another malignancy.
Discussion: Hematemesis and hematochezia in patients with cirrhosis would be unlikely to raise suspicion for amyloidosis. Endoscopic visualization of gastric mucosa can capture rarer etiologies of GI bleeding such as AL amyloidosis which expands workup beyond the affected organ. GI amyloidosis presents systemically more often than localized. While systemic disease is managed with chemo/immunotherapy and/or hematopoietic cell transplant, localized GI amyloidosis continues to be a rare disease without specific guidelines for management.

Figure: A) Amyloid deposits on biopsy stained with H&E. B) Congo red staining. C & D) Apple green birefringence.
Disclosures:
Neel Matiwala indicated no relevant financial relationships.
Rohan Tripathi indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Ameya deshmukh indicated no relevant financial relationships.
Jay Shah indicated no relevant financial relationships.
Abdallah El Alayli indicated no relevant financial relationships.
Maya Mahmoud indicated no relevant financial relationships.
Eyad Gharaibeh indicated no relevant financial relationships.
Jennifer Palagiri indicated no relevant financial relationships.
Neel Matiwala, BS, Rohan Tripathi, BS, Hayden Rotramel, MD, Ameya deshmukh, DO, Jay Shah, DO, Abdallah El Alayli, MD, Maya Mahmoud, MD, Eyad Gharaibeh, MD, Jennifer Palagiri, MD. P2108 - Gastric Amyloidosis: A Rare Cause of Hematemesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

