Monday Poster Session
Category: Esophagus
P1902 - Not All White is Candida! Herpes Esophagitis Mimicking Esophageal Candidiasis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Amit Sah, MD
University of Miami at JFK Medical Center
Lantana, FL
Presenting Author(s)
Amit Sah, MD1, Rukmoni Balasubramanian, MBBS2, Laura Suzanne Suarez, MD2, Gregory Churchill, MD2, Ron Schey, MD3
1University of Miami at JFK Medical Center, Lantana, FL; 2University of Florida Jacksonville, Jacksonville, FL; 3University of Florida-Jacksonville, Jacksonville, FL
Introduction: Infectious esophagitis is the third most common cause of esophagitis. It is usually seen in immunocompromised individuals. Causative agents are Candida, CMV, or HSV. Diagnosis is often obvious during endoscopy however we present a patient with esophagogastroduodenoscopy (EGD) suggestive of candidiasis but with histopathology confirmative of herpetic esophagitis (HE). We will discuss the various atypical presentations and endoscopic appearances of HSV.
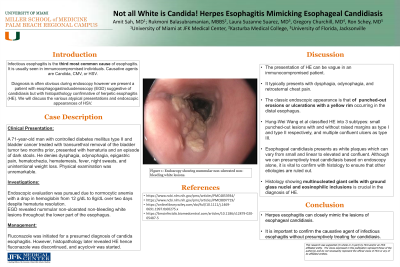
Case Description/Methods: A 71-year-old man with controlled diabetes mellitus type II and bladder cancer treated with transurethral removal of the bladder tumor two months prior, presented with hematuria and an episode of dark stools. He denies dysphagia, odynophagia, epigastric pain, hematochezia, hematemesis, fever, night sweats, and unintentional weight loss. Physical examination was unremarkable. Endoscopic evaluation was pursued due to normocytic anemia with a drop in hemoglobin from 12 g/dL to 8g/dL over two days despite hematuria resolution. EGD revealed nummular non-ulcerated non-bleeding white lesions throughout the lower part of the esophagus. Fluconazole was initiated for a presumed diagnosis of candida esophagitis. However, histopathology later revealed HE hence fluconazole was discontinued, and acyclovir was started.
Discussion: The presentation of HE can be vague in an immunocompromised patient. It typically presents with dysphagia, odynophagia, and retrosternal chest pain with a classic endoscopic appearance of punched-out erosions or ulcerations with a yellow rim occurring in the distal esophagus. Hung-Wei Wang et al classified HE into 3 subtypes: small punched-out lesions with and without raised margins as type I and type II respectively, and multiple confluent ulcers as type III. Esophageal candidiasis presents as white plaques which can vary from small and linear to elevated and confluent. Although we can presumptively treat candidiasis based on endoscopy alone, it is vital to confirm with histology to ensure that other etiologies are ruled out. Histology showing multinucleated giant cells with ground glass nuclei and eosinophilic inclusions is crucial in the diagnosis of HE.

Disclosures:
Amit Sah, MD1, Rukmoni Balasubramanian, MBBS2, Laura Suzanne Suarez, MD2, Gregory Churchill, MD2, Ron Schey, MD3. P1902 - Not All White is Candida! Herpes Esophagitis Mimicking Esophageal Candidiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Miami at JFK Medical Center, Lantana, FL; 2University of Florida Jacksonville, Jacksonville, FL; 3University of Florida-Jacksonville, Jacksonville, FL
Introduction: Infectious esophagitis is the third most common cause of esophagitis. It is usually seen in immunocompromised individuals. Causative agents are Candida, CMV, or HSV. Diagnosis is often obvious during endoscopy however we present a patient with esophagogastroduodenoscopy (EGD) suggestive of candidiasis but with histopathology confirmative of herpetic esophagitis (HE). We will discuss the various atypical presentations and endoscopic appearances of HSV.
Case Description/Methods: A 71-year-old man with controlled diabetes mellitus type II and bladder cancer treated with transurethral removal of the bladder tumor two months prior, presented with hematuria and an episode of dark stools. He denies dysphagia, odynophagia, epigastric pain, hematochezia, hematemesis, fever, night sweats, and unintentional weight loss. Physical examination was unremarkable. Endoscopic evaluation was pursued due to normocytic anemia with a drop in hemoglobin from 12 g/dL to 8g/dL over two days despite hematuria resolution. EGD revealed nummular non-ulcerated non-bleeding white lesions throughout the lower part of the esophagus. Fluconazole was initiated for a presumed diagnosis of candida esophagitis. However, histopathology later revealed HE hence fluconazole was discontinued, and acyclovir was started.
Discussion: The presentation of HE can be vague in an immunocompromised patient. It typically presents with dysphagia, odynophagia, and retrosternal chest pain with a classic endoscopic appearance of punched-out erosions or ulcerations with a yellow rim occurring in the distal esophagus. Hung-Wei Wang et al classified HE into 3 subtypes: small punched-out lesions with and without raised margins as type I and type II respectively, and multiple confluent ulcers as type III. Esophageal candidiasis presents as white plaques which can vary from small and linear to elevated and confluent. Although we can presumptively treat candidiasis based on endoscopy alone, it is vital to confirm with histology to ensure that other etiologies are ruled out. Histology showing multinucleated giant cells with ground glass nuclei and eosinophilic inclusions is crucial in the diagnosis of HE.

Figure: Endoscopy showing plaque like lesion in the middle third esophagus
Disclosures:
Amit Sah indicated no relevant financial relationships.
Rukmoni Balasubramanian indicated no relevant financial relationships.
Laura Suzanne Suarez indicated no relevant financial relationships.
Gregory Churchill indicated no relevant financial relationships.
Ron Schey indicated no relevant financial relationships.
Amit Sah, MD1, Rukmoni Balasubramanian, MBBS2, Laura Suzanne Suarez, MD2, Gregory Churchill, MD2, Ron Schey, MD3. P1902 - Not All White is Candida! Herpes Esophagitis Mimicking Esophageal Candidiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
