Monday Poster Session
Category: Esophagus
P1905 - Unveiling the Enigmatic Lymphocytic Esophagitis: A Case Report Highlighting Clinical Variability and Endoscopic Manifestations
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- KS
Karan Sachdeva, MD
Louisiana State University Health
Shreveport, Louisiana
Presenting Author(s)
Karan Sachdeva, MD1, Nazar Hafiz, MD2, Bohdan Zoshchuk, MD3, David Okuampa, MD2, Sudha Pandit, MD2
1Louisiana State University Health, Shreveport, LA; 2LSU Health Sciences Center, Shreveport, LA; 3Louisiana State University Health Science, Shreveport, LA
Introduction: Lymphocytic esophagitis (LE) is a unique and atypical form of chronic esophagitis characterized by distinct clinical, histologic, and endoscopic features. It is more commonly seen in females over the age of 50 years, often presenting with a primary symptom of dysphagia. Unlike gastroesophageal reflux disease (GERD), which predominately affects the distal esophagus, LE is a disease that can manifest throughout the length of the tubular esophagus. The diagnosis of LE requires intraepithelial lymphocytosis without significant granulocytic inflammation and some evidence of epithelial damage such as basal zone hyperplasia, spongiosis, and/or dyskeratotic keratinocytes. The endoscopic features of LE can vary significantly and sometimes overlap with EoE (eosinophilic esophagitis) including esophageal strictures, edema, rings, furrows, and/or white plaques.
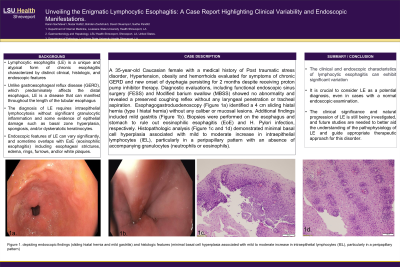
Case Description/Methods: A 35-year-old Caucasian female with a medical history of Post-traumatic stress disorder, Hypertension, obesity, and hemorrhoids was evaluated for symptoms of chronic GERD refractory to proton pump inhibitor therapy and new onset of dysphagia persisting for 2 months. Diagnostic evaluations, including functional endoscopic sinus surgery (FESS) and Modified barium swallow (MBSS) showed no abnormality and revealed a preserved coughing reflex without any laryngeal penetration or tracheal aspiration. Esophagogastroduodenoscopy (Figure 1a) identified a 4 cm sliding hiatal hernia (type I hiatal hernia) with mild distal esophagitis without any caliber or mucosal lesions. Biopsies were performed on the esophagus and stomach to rule out eosinophilic esophagitis (EoE) and H. Pylori infection, respectively. Histopathologic analysis (Figure 1b) demonstrated minimal basal cell hyperplasia associated with a mild to moderate increase in intraepithelial lymphocytes (IEL), particularly in a peri-papillary pattern with an absence of accompanying granulocytes (neutrophils or eosinophils).
Discussion: The clinical and endoscopic characteristics of lymphocytic esophagitis can exhibit significant variation. It is crucial to consider LE as a potential diagnosis, even in cases with a normal endoscopic examination. The clinical significance and natural progression of LE are still being investigated, and future studies are needed to better aid the understanding of the pathophysiology of LE and guide appropriate therapeutic approach for this disorder.

Disclosures:
Karan Sachdeva, MD1, Nazar Hafiz, MD2, Bohdan Zoshchuk, MD3, David Okuampa, MD2, Sudha Pandit, MD2. P1905 - Unveiling the Enigmatic Lymphocytic Esophagitis: A Case Report Highlighting Clinical Variability and Endoscopic Manifestations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Louisiana State University Health, Shreveport, LA; 2LSU Health Sciences Center, Shreveport, LA; 3Louisiana State University Health Science, Shreveport, LA
Introduction: Lymphocytic esophagitis (LE) is a unique and atypical form of chronic esophagitis characterized by distinct clinical, histologic, and endoscopic features. It is more commonly seen in females over the age of 50 years, often presenting with a primary symptom of dysphagia. Unlike gastroesophageal reflux disease (GERD), which predominately affects the distal esophagus, LE is a disease that can manifest throughout the length of the tubular esophagus. The diagnosis of LE requires intraepithelial lymphocytosis without significant granulocytic inflammation and some evidence of epithelial damage such as basal zone hyperplasia, spongiosis, and/or dyskeratotic keratinocytes. The endoscopic features of LE can vary significantly and sometimes overlap with EoE (eosinophilic esophagitis) including esophageal strictures, edema, rings, furrows, and/or white plaques.
Case Description/Methods: A 35-year-old Caucasian female with a medical history of Post-traumatic stress disorder, Hypertension, obesity, and hemorrhoids was evaluated for symptoms of chronic GERD refractory to proton pump inhibitor therapy and new onset of dysphagia persisting for 2 months. Diagnostic evaluations, including functional endoscopic sinus surgery (FESS) and Modified barium swallow (MBSS) showed no abnormality and revealed a preserved coughing reflex without any laryngeal penetration or tracheal aspiration. Esophagogastroduodenoscopy (Figure 1a) identified a 4 cm sliding hiatal hernia (type I hiatal hernia) with mild distal esophagitis without any caliber or mucosal lesions. Biopsies were performed on the esophagus and stomach to rule out eosinophilic esophagitis (EoE) and H. Pylori infection, respectively. Histopathologic analysis (Figure 1b) demonstrated minimal basal cell hyperplasia associated with a mild to moderate increase in intraepithelial lymphocytes (IEL), particularly in a peri-papillary pattern with an absence of accompanying granulocytes (neutrophils or eosinophils).
Discussion: The clinical and endoscopic characteristics of lymphocytic esophagitis can exhibit significant variation. It is crucial to consider LE as a potential diagnosis, even in cases with a normal endoscopic examination. The clinical significance and natural progression of LE are still being investigated, and future studies are needed to better aid the understanding of the pathophysiology of LE and guide appropriate therapeutic approach for this disorder.

Figure: Figure 1. Depicting endoscopic and histopathological findings.
Disclosures:
Karan Sachdeva indicated no relevant financial relationships.
Nazar Hafiz indicated no relevant financial relationships.
Bohdan Zoshchuk indicated no relevant financial relationships.
David Okuampa indicated no relevant financial relationships.
Sudha Pandit indicated no relevant financial relationships.
Karan Sachdeva, MD1, Nazar Hafiz, MD2, Bohdan Zoshchuk, MD3, David Okuampa, MD2, Sudha Pandit, MD2. P1905 - Unveiling the Enigmatic Lymphocytic Esophagitis: A Case Report Highlighting Clinical Variability and Endoscopic Manifestations, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
