Monday Poster Session
Category: Esophagus
P1914 - Esophagitis Dissecans Superficialis in an Immunocompromised Patient - Not All White Plaques Are Candida
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Justice Arhinful, MD
Howard University Hospital
Washington, DC
Presenting Author(s)
Justice Arhinful, MD, Abdullahi Musa, MD, Temitayo Gboluaje, MD, Chineduu Okeke, MD, Olanrewaju Oni, MD, Mica Grantham, MD, Laiyemo Adeyinka, MD, MPH, FACG
Howard University Hospital, Washington, DC
Introduction: Esophagitis Dissecans Superficialis (EDS) is a rare endoscopic finding characterized by sloughing and desquamation of large fragments of the superficial esophageal mucosa. In spite of its dramatic endoscopic appearance, EDS is known to be benign and usually resolves with no sequelae. However, it can easily be misidentified as a fungal esophagitis in an immunosuppressed patient. We report a case of EDS with concurrent gastro-jejunal anastomotic ulceration in an immunocompromised patient who presented with GI bleeding.
Case Description/Methods: A 42-year-old African American male with history of perforated peptic ulcer disease, gastric bypass surgery and recently diagnosed HIV (not on HAART) presented with a 2-week history of worsening fatigue and shortness of breath in the setting of dark tarry stools. He denied any abdominal pain but endorsed anorexia, lightheadedness, and recent weight loss. His hemoglobin was 6.9 g/dL for which he was transfused 1 unit of packed red cells. He was started on empiric pantoprazole 40 mg BID. EGD revealed superficial ulceration at the gastro-jejunal anastomotic site and severe esophagitis with strips of peeling whitish esophageal mucosa involving the middle and distal esophagus concerning for candida esophagitis. However, multiple esophageal biopsies showed squamous epithelium with detached parakeratotic layer, necrotic debris and bacterial colonies with features suggestive for esophagitis dissecans superficialis; fungal staining was negative. Symptoms improved with PPI.
Discussion: EDS is a rare but benign desquamative esophageal condition which could be idiopathic or associated with certain chemical irritants, medications such as bisphosphonates, esophageal strictures, celiac disease, immunosuppressed states or autoimmune conditions. Clinically, some patients complain of longstanding dysphagia, while others, like our patient, report no esophageal symptoms. In spite of the above associations, most cases of EDS remain unexplained, and the histopathologic features of EDS have not been adequately described. EDS is characterized endoscopically by sloughing of the mucosal layer which can easily be confused with candidal esophagitis especially in the setting of immunosuppression. Clinicians must therefore rely on esophageal biopsies to confirm diagnosis. Our case emphasizes the importance of considering EDS as a differential diagnosis during interpretation of whitish esophageal lesions in an immunocompromised patient in order to avoid unwarranted antifungal therapy.

Disclosures:
Justice Arhinful, MD, Abdullahi Musa, MD, Temitayo Gboluaje, MD, Chineduu Okeke, MD, Olanrewaju Oni, MD, Mica Grantham, MD, Laiyemo Adeyinka, MD, MPH, FACG. P1914 - Esophagitis Dissecans Superficialis in an Immunocompromised Patient - Not All White Plaques Are Candida, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Howard University Hospital, Washington, DC
Introduction: Esophagitis Dissecans Superficialis (EDS) is a rare endoscopic finding characterized by sloughing and desquamation of large fragments of the superficial esophageal mucosa. In spite of its dramatic endoscopic appearance, EDS is known to be benign and usually resolves with no sequelae. However, it can easily be misidentified as a fungal esophagitis in an immunosuppressed patient. We report a case of EDS with concurrent gastro-jejunal anastomotic ulceration in an immunocompromised patient who presented with GI bleeding.
Case Description/Methods: A 42-year-old African American male with history of perforated peptic ulcer disease, gastric bypass surgery and recently diagnosed HIV (not on HAART) presented with a 2-week history of worsening fatigue and shortness of breath in the setting of dark tarry stools. He denied any abdominal pain but endorsed anorexia, lightheadedness, and recent weight loss. His hemoglobin was 6.9 g/dL for which he was transfused 1 unit of packed red cells. He was started on empiric pantoprazole 40 mg BID. EGD revealed superficial ulceration at the gastro-jejunal anastomotic site and severe esophagitis with strips of peeling whitish esophageal mucosa involving the middle and distal esophagus concerning for candida esophagitis. However, multiple esophageal biopsies showed squamous epithelium with detached parakeratotic layer, necrotic debris and bacterial colonies with features suggestive for esophagitis dissecans superficialis; fungal staining was negative. Symptoms improved with PPI.
Discussion: EDS is a rare but benign desquamative esophageal condition which could be idiopathic or associated with certain chemical irritants, medications such as bisphosphonates, esophageal strictures, celiac disease, immunosuppressed states or autoimmune conditions. Clinically, some patients complain of longstanding dysphagia, while others, like our patient, report no esophageal symptoms. In spite of the above associations, most cases of EDS remain unexplained, and the histopathologic features of EDS have not been adequately described. EDS is characterized endoscopically by sloughing of the mucosal layer which can easily be confused with candidal esophagitis especially in the setting of immunosuppression. Clinicians must therefore rely on esophageal biopsies to confirm diagnosis. Our case emphasizes the importance of considering EDS as a differential diagnosis during interpretation of whitish esophageal lesions in an immunocompromised patient in order to avoid unwarranted antifungal therapy.

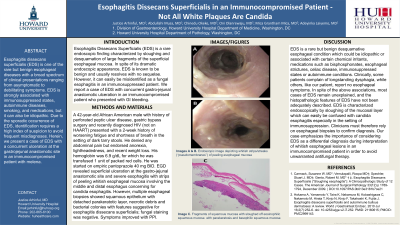
Figure: Images A & B showing endoscopic photograph of the esophagus depicting whitish strips or streaks (‘‘pseudomembranes’’) of peeling esophageal mucosa during an endoscopic examination
Image C depicts medium magnification showing two fragments of squamous mucosa showing sloughed off eosinophilic squamous mucosa with parakeratosis and basophilic squamous mucosa
Image C depicts medium magnification showing two fragments of squamous mucosa showing sloughed off eosinophilic squamous mucosa with parakeratosis and basophilic squamous mucosa
Disclosures:
Justice Arhinful indicated no relevant financial relationships.
Abdullahi Musa indicated no relevant financial relationships.
Temitayo Gboluaje indicated no relevant financial relationships.
Chineduu Okeke indicated no relevant financial relationships.
Olanrewaju Oni indicated no relevant financial relationships.
Mica Grantham indicated no relevant financial relationships.
Laiyemo Adeyinka indicated no relevant financial relationships.
Justice Arhinful, MD, Abdullahi Musa, MD, Temitayo Gboluaje, MD, Chineduu Okeke, MD, Olanrewaju Oni, MD, Mica Grantham, MD, Laiyemo Adeyinka, MD, MPH, FACG. P1914 - Esophagitis Dissecans Superficialis in an Immunocompromised Patient - Not All White Plaques Are Candida, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
