Monday Poster Session
Category: Colon
P1720 - Colonic Histoplasmosis: A Rare Cause of Diarrhea in an Immunocompromised Patient Which Is Often Late to Be Diagnosed
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AP
Arsheya Patel, MD
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Arsheya Patel, MD, Waqas Nawaz, MD
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Histoplasmosis is the most common endemic mycosis in the Ohio and Mississippi River Valley. Though most infections are asymptomatic, patients with compromised cellular immunity, such as those who undergo solid organ transplant, are at risk for disseminated disease. Symptomatic gastrointestinal (GI) involvement in disseminated histoplasmosis is rare and typically diagnosed in only 3-12% of cases. We describe a case of a solid organ transplant recipient who presented with fevers and acute diarrhea secondary to GI histoplasmosis.
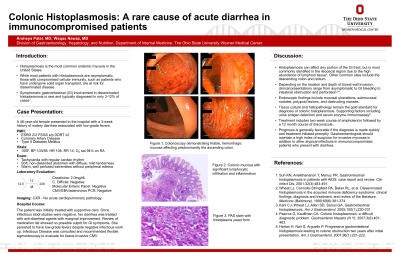
Case Description/Methods: A 46-year-old female presented to the hospital with a 3-week history of watery diarrhea associated with low-grade fevers. She had a history of end-stage renal disease secondary to focal segmental glomerulosclerosis requiring renal transplant two years prior to presentation. She took tacrolimus and mycophenolate for immunosuppression, but denied any regular NSAID use, recent sick contacts, or travel. Physical exam was unremarkable. Laboratory evaluation including infectious stool studies, CMV, EBV, and adenovirus PCR were negative. She underwent a diagnostic colonoscopy which demonstrated extensive friability and hemorrhagic petechiae all throughout the colon. The terminal ileum could not be intubated due to significant ileocecal valve edema. Colonic biopsies revealed mucosa with yeast forms morphologically consistent with Histoplasma spp. She was subsequently found to have a positive serum and urine Histoplasma antigen as well as Histoplasma fungemia consistent with disseminated histoplasmosis. She was started on amphotericin with prompt resolution of fevers and improvement in her diarrhea. After a 2-week course, she was transitioned to itraconazole. Upon discharge, she had complete resolution of all presenting symptoms.
Discussion: GI histoplasmosis is an infrequent clinical entity with a myriad of presentations. Histoplasma can be found anywhere in the GI tract, but most commonly affects the ileocecal region due to the abundance of lymphoid tissue in this area4. Depending on the location of bowel involved, symptoms include abdominal pain, diarrhea, bleeding, intestinal obstruction, and perforation5. Endoscopic findings range from mucosal ulcerations mimicking inflammatory bowel disease to submucosal nodules and polypoid lesions imitating malignancy3. A high index of suspicion is required to make the diagnosis and prompt recognition of the disease can significantly limit patient morbidity and mortality.

Disclosures:
Arsheya Patel, MD, Waqas Nawaz, MD. P1720 - Colonic Histoplasmosis: A Rare Cause of Diarrhea in an Immunocompromised Patient Which Is Often Late to Be Diagnosed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Histoplasmosis is the most common endemic mycosis in the Ohio and Mississippi River Valley. Though most infections are asymptomatic, patients with compromised cellular immunity, such as those who undergo solid organ transplant, are at risk for disseminated disease. Symptomatic gastrointestinal (GI) involvement in disseminated histoplasmosis is rare and typically diagnosed in only 3-12% of cases. We describe a case of a solid organ transplant recipient who presented with fevers and acute diarrhea secondary to GI histoplasmosis.
Case Description/Methods: A 46-year-old female presented to the hospital with a 3-week history of watery diarrhea associated with low-grade fevers. She had a history of end-stage renal disease secondary to focal segmental glomerulosclerosis requiring renal transplant two years prior to presentation. She took tacrolimus and mycophenolate for immunosuppression, but denied any regular NSAID use, recent sick contacts, or travel. Physical exam was unremarkable. Laboratory evaluation including infectious stool studies, CMV, EBV, and adenovirus PCR were negative. She underwent a diagnostic colonoscopy which demonstrated extensive friability and hemorrhagic petechiae all throughout the colon. The terminal ileum could not be intubated due to significant ileocecal valve edema. Colonic biopsies revealed mucosa with yeast forms morphologically consistent with Histoplasma spp. She was subsequently found to have a positive serum and urine Histoplasma antigen as well as Histoplasma fungemia consistent with disseminated histoplasmosis. She was started on amphotericin with prompt resolution of fevers and improvement in her diarrhea. After a 2-week course, she was transitioned to itraconazole. Upon discharge, she had complete resolution of all presenting symptoms.
Discussion: GI histoplasmosis is an infrequent clinical entity with a myriad of presentations. Histoplasma can be found anywhere in the GI tract, but most commonly affects the ileocecal region due to the abundance of lymphoid tissue in this area4. Depending on the location of bowel involved, symptoms include abdominal pain, diarrhea, bleeding, intestinal obstruction, and perforation5. Endoscopic findings range from mucosal ulcerations mimicking inflammatory bowel disease to submucosal nodules and polypoid lesions imitating malignancy3. A high index of suspicion is required to make the diagnosis and prompt recognition of the disease can significantly limit patient morbidity and mortality.

Figure: Friable cecum with edematous ileocecal valve in the setting of colonic histoplasmosis.
Disclosures:
Arsheya Patel indicated no relevant financial relationships.
Waqas Nawaz indicated no relevant financial relationships.
Arsheya Patel, MD, Waqas Nawaz, MD. P1720 - Colonic Histoplasmosis: A Rare Cause of Diarrhea in an Immunocompromised Patient Which Is Often Late to Be Diagnosed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
