Monday Poster Session
Category: Colon
P1722 - When it Is Not Adenocarcinoma: Primary Squamous Cell Carcinoma of the Ascending Colon Presenting as Unexplained Iron Deficiency Anemia
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Farhan Azad, DO
University at Buffalo
Buffalo, New York
Presenting Author(s)
Award: Presidential Poster Award
Farhan Azad, DO, Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Ross R. Moyer, DO, Prutha Patel, DO, Eric J. Dove, MD, Muddasir Ayaz, MD
University at Buffalo, Buffalo, NY
Introduction: Squamous cell carcinoma of the colon (SCCC) represents 0.1 to 0.5% of colorectal cancer cases worldwide. The etiology is unclear, although it is hypothesized to be originating from a multipotent stem cell and developing metaplasia from chronic inflammation or irritation. Compared to adenocarcinoma of the colon (ACC), it is often diagnosed late and has a poor prognosis.
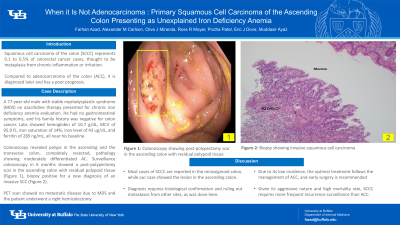
Case Description/Methods: A 77-year-old male with a history of myelodysplastic syndrome (MDS) on azacitidine therapy presented for an endoscopic evaluation of chronic iron deficiency anemia. He denied any nausea, vomiting, abdominal pain, diarrhea, constipation, or any blood in the stool. His family history was negative for colon cancer. The patient was hemodynamically stable. On exam, the abdomen was soft, non-distended, and non-tender to palpation. Laboratory values revealed hemoglobin of 10.7 g/dL, MCV of 95.9 fL, iron saturation of 14%, iron level of 43 ug/dL, and ferritin of 289 ng/mL, all near his baseline. Colonoscopy revealed a polyp in the ascending and transverse colon, both resected and retrieved, with pathology showing moderately differentiated adenocarcinoma. There was no evidence of active bleeding in the colon and other tumors or masses. It was thought that the ACC was confined to the polyp and completely resected. A surveillance colonoscopy 6 months later revealed a post-polypectomy scar in the ascending colon with residual polypoid tissue which was biopsied (Figure 1). Biopsy revealed a new invasive squamous cell carcinoma (Figure 2). Immunohistochemistry (IHC) showed positive cytokeratin 5/6, P40, and cytokeratin 20. IHC was negative for cytokeratin 7 and CDX-2. PET scan revealed uptake in the bone marrow without definite CT scan correlates, related to the patient’s MDS, with no evidence of metastatic disease. He was scheduled for a right hemicolectomy, with plans to hold the preceding cycle of chemotherapy to allow for surgery.
Discussion: Most cases of SCCC are reported in the rectosigmoid colon, while our case showed the lesion in the ascending colon. The diagnosis requires histological confirmation and ruling out metastases from other sites, as was done here. Due to its low incidence, the optimal treatment follows the management of ACC and early surgery is the first step in reducing the high mortality rate. Given its aggressive nature, SCCC requires more frequent recurrence surveillance than ACC. The case highlights the need for a multidisciplinary approach in these patients.

Disclosures:
Farhan Azad, DO, Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Ross R. Moyer, DO, Prutha Patel, DO, Eric J. Dove, MD, Muddasir Ayaz, MD. P1722 - When it Is Not Adenocarcinoma: Primary Squamous Cell Carcinoma of the Ascending Colon Presenting as Unexplained Iron Deficiency Anemia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Farhan Azad, DO, Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Ross R. Moyer, DO, Prutha Patel, DO, Eric J. Dove, MD, Muddasir Ayaz, MD
University at Buffalo, Buffalo, NY
Introduction: Squamous cell carcinoma of the colon (SCCC) represents 0.1 to 0.5% of colorectal cancer cases worldwide. The etiology is unclear, although it is hypothesized to be originating from a multipotent stem cell and developing metaplasia from chronic inflammation or irritation. Compared to adenocarcinoma of the colon (ACC), it is often diagnosed late and has a poor prognosis.
Case Description/Methods: A 77-year-old male with a history of myelodysplastic syndrome (MDS) on azacitidine therapy presented for an endoscopic evaluation of chronic iron deficiency anemia. He denied any nausea, vomiting, abdominal pain, diarrhea, constipation, or any blood in the stool. His family history was negative for colon cancer. The patient was hemodynamically stable. On exam, the abdomen was soft, non-distended, and non-tender to palpation. Laboratory values revealed hemoglobin of 10.7 g/dL, MCV of 95.9 fL, iron saturation of 14%, iron level of 43 ug/dL, and ferritin of 289 ng/mL, all near his baseline. Colonoscopy revealed a polyp in the ascending and transverse colon, both resected and retrieved, with pathology showing moderately differentiated adenocarcinoma. There was no evidence of active bleeding in the colon and other tumors or masses. It was thought that the ACC was confined to the polyp and completely resected. A surveillance colonoscopy 6 months later revealed a post-polypectomy scar in the ascending colon with residual polypoid tissue which was biopsied (Figure 1). Biopsy revealed a new invasive squamous cell carcinoma (Figure 2). Immunohistochemistry (IHC) showed positive cytokeratin 5/6, P40, and cytokeratin 20. IHC was negative for cytokeratin 7 and CDX-2. PET scan revealed uptake in the bone marrow without definite CT scan correlates, related to the patient’s MDS, with no evidence of metastatic disease. He was scheduled for a right hemicolectomy, with plans to hold the preceding cycle of chemotherapy to allow for surgery.
Discussion: Most cases of SCCC are reported in the rectosigmoid colon, while our case showed the lesion in the ascending colon. The diagnosis requires histological confirmation and ruling out metastases from other sites, as was done here. Due to its low incidence, the optimal treatment follows the management of ACC and early surgery is the first step in reducing the high mortality rate. Given its aggressive nature, SCCC requires more frequent recurrence surveillance than ACC. The case highlights the need for a multidisciplinary approach in these patients.

Figure: Figure 1: Colonoscopy showing post-polypectomy scar in the ascending colon with residual polypoid tissue
Figure 2: Biopsy showing invasive squamous cell carcinoma
Figure 2: Biopsy showing invasive squamous cell carcinoma
Disclosures:
Farhan Azad indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Ross Moyer indicated no relevant financial relationships.
Prutha Patel indicated no relevant financial relationships.
Eric Dove indicated no relevant financial relationships.
Muddasir Ayaz indicated no relevant financial relationships.
Farhan Azad, DO, Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Ross R. Moyer, DO, Prutha Patel, DO, Eric J. Dove, MD, Muddasir Ayaz, MD. P1722 - When it Is Not Adenocarcinoma: Primary Squamous Cell Carcinoma of the Ascending Colon Presenting as Unexplained Iron Deficiency Anemia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

