Monday Poster Session
Category: Biliary/Pancreas
P1493 - Pancreatic Mesothelial Cyst Diagnosed via Endoscopic Ultrasound-Guided Fine Needle Aspiration and Through-The-Needle Biopsy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ramon O. Minjares, MD
Underwood Center for Digestive Disorders, Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Ramon O. Minjares, MD1, Shaadi Abughazaleh, MD2, Patrick R. Reardon, MD2, Michael Deavers, MD2, Blythe Gorman, MD2, Alberto O. Barroso, MD3
1Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX; 2Houston Methodist Hospital, Houston, TX; 3Houston Methodist Research Institute and Weill Cornell College of Medicine, Houston, TX
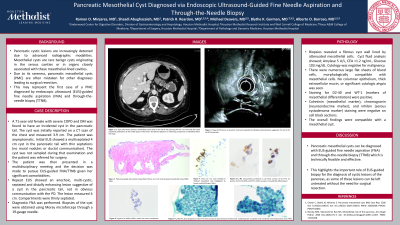
Introduction: Pancreatic cystic lesions are increasingly detected due to advanced radiographic modalities. Mesothelial cysts are rare benign cysts originating in the serous cavities or in organs closely associated with these mesothelial-lined cavities. Due to its rareness, pancreatic mesothelial cyst (PMC) is often mistaken for other diagnoses leading to surgical resection. This may represent the first case of a PMC diagnosed by endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) and through-the-needle biopsy (TTNB).
Case Description/Methods: A 71-year-old female with severe COPD and DM was found to have an incidental cyst in the pancreatic tail. The cyst was initially reported on a CT scan of the chest and measured 3.9 cm. The patient was completely asymptomatic. Initial EUS showed a multiseptated 4 cm cyst in the pancreatic tail with thin septations (no mural nodules or ductal communication). The cyst was not sampled during that examination and the patient was referred for surgery. The patient was presented in our multidisciplinary meeting and the decision was made to pursue EUS-guided FNA/TTNB given her significant comorbidities.
Repeat EUS showed an anechoic, multi-cystic, septated and distally enhancing lesion suggestive of a cyst in the pancreatic tail, not in obvious communication with the PD. The lesion measured 4 cm. Compartments were thinly septated. Diagnostic FNA was performed. Biopsies of the cyst were obtained using microforceps (Moray) through a 19-gauge needle.
Biopsies revealed a fibrous cyst wall lined by attenuated mesothelial cells. Cyst fluid analysis showed Amylase 5 U/L, CEA < 1.2 ng/mL, Glucose 103 mg/dL. Cytology was negative for malignancy. There were numerous large flat sheets of bland cells, morphologically compatible with mesothelial cells. No columnar epithelium, thick extracellular mucin, or significant cytologic atypia was seen. Staining for D2-40 and WT-1 (markers of mesothelial differentiation) were positive. Calretinin (mesothelial marker), chromogranin (neuroendocrine marker), and inhibin (serous cystadenoma marker) staining were negative on cell block sections. The overall findings were compatible with a mesothelial cyst.
Discussion: PMC can be diagnosed with EUS-guided FNA/TTNB which is technically feasible and effective. This highlights the important role of EUS-guided biopsy for the diagnosis of cystic lesions of the pancreas as some of these lesions can be left untreated without the need for surgical resection.

Disclosures:
Ramon O. Minjares, MD1, Shaadi Abughazaleh, MD2, Patrick R. Reardon, MD2, Michael Deavers, MD2, Blythe Gorman, MD2, Alberto O. Barroso, MD3. P1493 - Pancreatic Mesothelial Cyst Diagnosed via Endoscopic Ultrasound-Guided Fine Needle Aspiration and Through-The-Needle Biopsy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX; 2Houston Methodist Hospital, Houston, TX; 3Houston Methodist Research Institute and Weill Cornell College of Medicine, Houston, TX
Introduction: Pancreatic cystic lesions are increasingly detected due to advanced radiographic modalities. Mesothelial cysts are rare benign cysts originating in the serous cavities or in organs closely associated with these mesothelial-lined cavities. Due to its rareness, pancreatic mesothelial cyst (PMC) is often mistaken for other diagnoses leading to surgical resection. This may represent the first case of a PMC diagnosed by endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) and through-the-needle biopsy (TTNB).
Case Description/Methods: A 71-year-old female with severe COPD and DM was found to have an incidental cyst in the pancreatic tail. The cyst was initially reported on a CT scan of the chest and measured 3.9 cm. The patient was completely asymptomatic. Initial EUS showed a multiseptated 4 cm cyst in the pancreatic tail with thin septations (no mural nodules or ductal communication). The cyst was not sampled during that examination and the patient was referred for surgery. The patient was presented in our multidisciplinary meeting and the decision was made to pursue EUS-guided FNA/TTNB given her significant comorbidities.
Repeat EUS showed an anechoic, multi-cystic, septated and distally enhancing lesion suggestive of a cyst in the pancreatic tail, not in obvious communication with the PD. The lesion measured 4 cm. Compartments were thinly septated. Diagnostic FNA was performed. Biopsies of the cyst were obtained using microforceps (Moray) through a 19-gauge needle.
Biopsies revealed a fibrous cyst wall lined by attenuated mesothelial cells. Cyst fluid analysis showed Amylase 5 U/L, CEA < 1.2 ng/mL, Glucose 103 mg/dL. Cytology was negative for malignancy. There were numerous large flat sheets of bland cells, morphologically compatible with mesothelial cells. No columnar epithelium, thick extracellular mucin, or significant cytologic atypia was seen. Staining for D2-40 and WT-1 (markers of mesothelial differentiation) were positive. Calretinin (mesothelial marker), chromogranin (neuroendocrine marker), and inhibin (serous cystadenoma marker) staining were negative on cell block sections. The overall findings were compatible with a mesothelial cyst.
Discussion: PMC can be diagnosed with EUS-guided FNA/TTNB which is technically feasible and effective. This highlights the important role of EUS-guided biopsy for the diagnosis of cystic lesions of the pancreas as some of these lesions can be left untreated without the need for surgical resection.

Figure: Figure 1A, 1B. CT scan (coronal and axial view) showed a well-defined cystic lesion in the tail of the pancreas that measures 49 mm x 37 mm with few small peripheral calcifications at the medial aspect of the lesion. No definite septations or enhancing component are identified within this lesion. There is no dilation of the pancreatic duct.
Disclosures:
Ramon Minjares indicated no relevant financial relationships.
Shaadi Abughazaleh indicated no relevant financial relationships.
Patrick Reardon indicated no relevant financial relationships.
Michael Deavers indicated no relevant financial relationships.
Blythe Gorman indicated no relevant financial relationships.
Alberto Barroso indicated no relevant financial relationships.
Ramon O. Minjares, MD1, Shaadi Abughazaleh, MD2, Patrick R. Reardon, MD2, Michael Deavers, MD2, Blythe Gorman, MD2, Alberto O. Barroso, MD3. P1493 - Pancreatic Mesothelial Cyst Diagnosed via Endoscopic Ultrasound-Guided Fine Needle Aspiration and Through-The-Needle Biopsy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
