Monday Poster Session
Category: Biliary/Pancreas
P1509 - The Six-Year Itch: Intrahepatic Cholangiocarcinoma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Lily Kuo, MD
University of Texas Health Science Center San Antonio
San Antonio, TX
Presenting Author(s)
Lily Kuo, MD1, Grace Hopp, DO, MBA2, Brooke Anliker, MD3, Lisa Pedicone, PhD4, Carmen Landaverde, MD5, Eric Lawitz, MD5, Jan Petrasek, MD, PhD6, Fred Poordad, MD5, Fabian Rodas, MD5, Eugenia Tsai, MD5
1University of Texas Health Science Center San Antonio, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX; 3University of Texas Health San Antonio, San Antonio, TX; 4Texas Liver Institute, San Antonio, TX; 5UT Health San Antonio, Texas Liver Institute, San Antonio, TX; 6UT Health San Antonio, Texas Liver Institute, Jackson, MS
Introduction: Intrahepatic cholangiocarcinoma (iCCA) is associated with high morbidity and mortality, with a 5-year survival rate of 15%. We present a case of iCCA that started with an atypical presentation of pruritus.
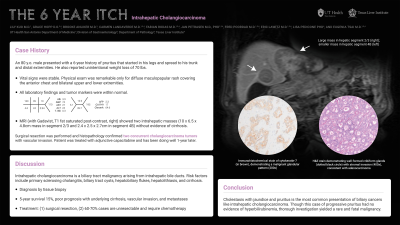
Case Description/Methods: An 80-year-old male with coronary artery disease and type 2 diabetes mellitus presented with 6 years of waxing and waning pruritus. The pruritus started on his legs, spread to his torso, and progressed to his hands and feet. Review of systems was significant for an unintentional 70-pound weight loss. Physical exam was notable for diffuse maculopapular rash on his chest and extremities. Full lab work up was normal. A contrast-enhanced CT of the abdomen and pelvis revealed two heterogenous liver masses. Further evaluation with MRI w/wo Gadavist demonstrated 10 x 6.5 x 4.8 cm hepatic segment II/III and 2.4 x 2.5 x 2.7 cm hepatic segment IVb masses (Figure 1a). Serum tumor markers were normal (alpha-fetoprotein 2.1 ng/dL, CA 19-9 16 U/mL). Histopathology from biopsies of the liver masses showed malignant cells staining positive for pancytokeratin and cytokeratin 7, consistent with adenocarcinoma of pancreaticobiliary origin (Figure 1b).
The patient underwent open partial hepatectomy of the left hepatic and caudate lobes. Surgical pathology confirmed sequential moderately-invasive iCCA with lymphovascular invasion. Adjuvant therapy with capacitabine was initiated for locally advanced disease. One year later, patient is clinically doing well and remains symptom-free.
Discussion: iCCA is a subclass of biliary tract malignancy arising from intrahepatic bile ducts. Risk factors for iCCA include primary sclerosing cholangitis, biliary tract cysts, hepatobiliary flukes, hepatolithiasis and cirrhosis. Diagnosis requires tissue biopsy. Surgical resection is considered first line therapy for early-stage disease with amenable anatomy, while advanced disease is managed with palliative chemotherapy. Local vascular invasion, metastasis, underlying cirrhosis, and the presence of sequential tumors are associated with worse prognosis.
Jaundice, typically a sign of cholestasis, is the most common manifestation of biliary cancers and can present with pruritus. Curiously, while our patient’s progressive pruritus was not associated with jaundice or hyperbilirubinemia, a thorough evaluation yielded a rare and fatal malignancy. This case highlights the importance of full investigation of all liver masses, even in the setting of nonspecific symptoms.

Disclosures:
Lily Kuo, MD1, Grace Hopp, DO, MBA2, Brooke Anliker, MD3, Lisa Pedicone, PhD4, Carmen Landaverde, MD5, Eric Lawitz, MD5, Jan Petrasek, MD, PhD6, Fred Poordad, MD5, Fabian Rodas, MD5, Eugenia Tsai, MD5. P1509 - The Six-Year Itch: Intrahepatic Cholangiocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center San Antonio, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX; 3University of Texas Health San Antonio, San Antonio, TX; 4Texas Liver Institute, San Antonio, TX; 5UT Health San Antonio, Texas Liver Institute, San Antonio, TX; 6UT Health San Antonio, Texas Liver Institute, Jackson, MS
Introduction: Intrahepatic cholangiocarcinoma (iCCA) is associated with high morbidity and mortality, with a 5-year survival rate of 15%. We present a case of iCCA that started with an atypical presentation of pruritus.
Case Description/Methods: An 80-year-old male with coronary artery disease and type 2 diabetes mellitus presented with 6 years of waxing and waning pruritus. The pruritus started on his legs, spread to his torso, and progressed to his hands and feet. Review of systems was significant for an unintentional 70-pound weight loss. Physical exam was notable for diffuse maculopapular rash on his chest and extremities. Full lab work up was normal. A contrast-enhanced CT of the abdomen and pelvis revealed two heterogenous liver masses. Further evaluation with MRI w/wo Gadavist demonstrated 10 x 6.5 x 4.8 cm hepatic segment II/III and 2.4 x 2.5 x 2.7 cm hepatic segment IVb masses (Figure 1a). Serum tumor markers were normal (alpha-fetoprotein 2.1 ng/dL, CA 19-9 16 U/mL). Histopathology from biopsies of the liver masses showed malignant cells staining positive for pancytokeratin and cytokeratin 7, consistent with adenocarcinoma of pancreaticobiliary origin (Figure 1b).
The patient underwent open partial hepatectomy of the left hepatic and caudate lobes. Surgical pathology confirmed sequential moderately-invasive iCCA with lymphovascular invasion. Adjuvant therapy with capacitabine was initiated for locally advanced disease. One year later, patient is clinically doing well and remains symptom-free.
Discussion: iCCA is a subclass of biliary tract malignancy arising from intrahepatic bile ducts. Risk factors for iCCA include primary sclerosing cholangitis, biliary tract cysts, hepatobiliary flukes, hepatolithiasis and cirrhosis. Diagnosis requires tissue biopsy. Surgical resection is considered first line therapy for early-stage disease with amenable anatomy, while advanced disease is managed with palliative chemotherapy. Local vascular invasion, metastasis, underlying cirrhosis, and the presence of sequential tumors are associated with worse prognosis.
Jaundice, typically a sign of cholestasis, is the most common manifestation of biliary cancers and can present with pruritus. Curiously, while our patient’s progressive pruritus was not associated with jaundice or hyperbilirubinemia, a thorough evaluation yielded a rare and fatal malignancy. This case highlights the importance of full investigation of all liver masses, even in the setting of nonspecific symptoms.

Figure: Figure 1. Liver masses consistent with intrahepatic cholangiocarcinoma: (a) Coronal view of MRI T1 fat saturated post-contrast showing two sequential heterogenous tumors in the liver; (b) Hematoxylin and eosin stain demonstrating well-formed cribiform glands (dotted black circle) with stromal invasion (400x magnification); (c) Immunohistochemical stain of cytokeratin-7 (in brown) in cytoplasm, demonstrating a malignant glandular pattern (200x magnification)
Disclosures:
Lily Kuo indicated no relevant financial relationships.
Grace Hopp indicated no relevant financial relationships.
Brooke Anliker indicated no relevant financial relationships.
Lisa Pedicone indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Eric Lawitz: 89Bio, Inc – Grant/Research Support. AbbVie – Grant/Research Support, Speakers Bureau. Akero – Advisor or Review Panel Member, Grant/Research Support. Allergan – Grant/Research Support. Alnylam – Grant/Research Support. Amgen – Grant/Research Support. Ascelia Pharma – Grant/Research Support. AstraZeneca – Grant/Research Support. Axcella Health – Grant/Research Support. Boehringer Ingelheim – Advisor or Review Panel Member, Grant/Research Support. Bristol Myers Squibb – Advisor or Review Panel Member, Grant/Research Support. Conatus Pharmaceuticals – Grant/Research Support. Cymabay – Grant/Research Support. CytoDyn – Grant/Research Support. DSM – Grant/Research Support. Durect Corporation – Grant/Research Support. Gilead – Speakers Bureau. Intercept – Advisor or Review Panel Member, Grant/Research Support, Speakers Bureau. Metacrine – Advisor or Review Panel Member. Novo Nordisk – Advisor or Review Panel Member. Sagimet – Advisor or Review Panel Member. Terns – Advisor or Review Panel Member.
Jan Petrasek indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Lily Kuo, MD1, Grace Hopp, DO, MBA2, Brooke Anliker, MD3, Lisa Pedicone, PhD4, Carmen Landaverde, MD5, Eric Lawitz, MD5, Jan Petrasek, MD, PhD6, Fred Poordad, MD5, Fabian Rodas, MD5, Eugenia Tsai, MD5. P1509 - The Six-Year Itch: Intrahepatic Cholangiocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
