Tuesday Poster Session
Category: IBD
P3687 - Incarcerated Parastomal Hernia in the Setting of Acute Rotavirus Infection in a Patient with Crohn’s Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Anastasia Chahine, MD
University of California Irvine
Orange, CA
Presenting Author(s)
Joshua Kwon, MD1, Anastasia Chahine, MD1, Amelie Tiritilli, MD2, Jason Samarasena, MD1, Robert Fearn, MD1, Valery vilchez, MD1
1University of California Irvine, Orange, CA; 2UC Irvine, Orange, CA
Introduction: Parastomal hernia formation after ileostomy is common, affecting 2-28% of end ileostomies. However, most affected patients are asymptomatic. Here we describe the case of a patient with Crohn's disease with colectomy and ileostomy creation complicated by an incarcerated parastomal hernia in the setting of an acute viral diarrheal illness.
Case Description/Methods: Patient is a 62-year-old male with a history of Crohn’s colitis status post total colectomy with end ileostomy due to multifocal low grade colonic dysplasia. Interval ileoscopy one year post-surgically showed no evidence of active inflammatory disease and the patient was doing well without the need for immunosuppressive therapy.
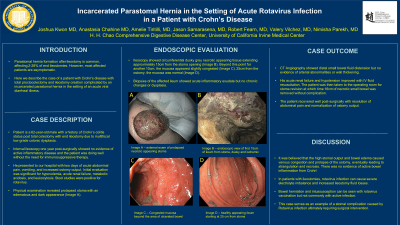
He presented to our hospital with two days of acute abdominal pain, vomiting, and increased ostomy output. Initial evaluation was significant for hypovolemia, acute renal failure, metabolic acidosis, and leukocytosis. Stool studies were positive for rotavirus. Physical examination revealed prolapsed stoma with an edematous and dark appearance (Image A). Ileoscopy showed circumferential dusky grey necrotic appearing tissue extending approximately 15cm from the stoma opening (Image B). Beyond this point for another 10cm, the mucosa appeared slightly congested (Image C). 25cm from the ostomy, the mucosa was normal (Image D). Biopsies of the affected ileum showed acute inflammatory exudate but no chronic changes or dysplasia.
CT Angiography showed distal small bowel fluid distension but no evidence of arterial abnormalities or wall thickening. His acute renal failure and hypotension improved with IV fluid resucitation. The patient was then taken to the operating room for stoma revision at which time 16cm of necrotic small bowel was removed without complication. The patient recovered well post-surgically with resolution of abdominal pain and normalization of ostomy output.
Discussion: It was believed that the high stomal output and bowel edema caused venous congestion and prolapse of the ostomy, eventually leading to strangulation and necrosis. There was no evidence of active Crohn’s disease causing bowel inflammation. In patients with ileostomies, rotavirus infection can cause severe electrolyte imbalance and increased ileostomy fluid losses. Bowel herniation and intussusception can be seen with rotavirus vaccination but not commonly with active infection. This case serves as an example of a stomal complication caused by Rotavirus infection ultimately requiring surgical intervention.

Disclosures:
Joshua Kwon, MD1, Anastasia Chahine, MD1, Amelie Tiritilli, MD2, Jason Samarasena, MD1, Robert Fearn, MD1, Valery vilchez, MD1. P3687 - Incarcerated Parastomal Hernia in the Setting of Acute Rotavirus Infection in a Patient with Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California Irvine, Orange, CA; 2UC Irvine, Orange, CA
Introduction: Parastomal hernia formation after ileostomy is common, affecting 2-28% of end ileostomies. However, most affected patients are asymptomatic. Here we describe the case of a patient with Crohn's disease with colectomy and ileostomy creation complicated by an incarcerated parastomal hernia in the setting of an acute viral diarrheal illness.
Case Description/Methods: Patient is a 62-year-old male with a history of Crohn’s colitis status post total colectomy with end ileostomy due to multifocal low grade colonic dysplasia. Interval ileoscopy one year post-surgically showed no evidence of active inflammatory disease and the patient was doing well without the need for immunosuppressive therapy.
He presented to our hospital with two days of acute abdominal pain, vomiting, and increased ostomy output. Initial evaluation was significant for hypovolemia, acute renal failure, metabolic acidosis, and leukocytosis. Stool studies were positive for rotavirus. Physical examination revealed prolapsed stoma with an edematous and dark appearance (Image A). Ileoscopy showed circumferential dusky grey necrotic appearing tissue extending approximately 15cm from the stoma opening (Image B). Beyond this point for another 10cm, the mucosa appeared slightly congested (Image C). 25cm from the ostomy, the mucosa was normal (Image D). Biopsies of the affected ileum showed acute inflammatory exudate but no chronic changes or dysplasia.
CT Angiography showed distal small bowel fluid distension but no evidence of arterial abnormalities or wall thickening. His acute renal failure and hypotension improved with IV fluid resucitation. The patient was then taken to the operating room for stoma revision at which time 16cm of necrotic small bowel was removed without complication. The patient recovered well post-surgically with resolution of abdominal pain and normalization of ostomy output.
Discussion: It was believed that the high stomal output and bowel edema caused venous congestion and prolapse of the ostomy, eventually leading to strangulation and necrosis. There was no evidence of active Crohn’s disease causing bowel inflammation. In patients with ileostomies, rotavirus infection can cause severe electrolyte imbalance and increased ileostomy fluid losses. Bowel herniation and intussusception can be seen with rotavirus vaccination but not commonly with active infection. This case serves as an example of a stomal complication caused by Rotavirus infection ultimately requiring surgical intervention.

Figure: A) External exam of prolapsed necrotic appearing stoma
B) Endoscopic view of first 15cm of ileum from stoma, dusky and ulcerated appearing
C) Congested mucosa beyond the area of ulcerated bowel
D) Healthy appearing ileum starting at 25 cm from stoma
B) Endoscopic view of first 15cm of ileum from stoma, dusky and ulcerated appearing
C) Congested mucosa beyond the area of ulcerated bowel
D) Healthy appearing ileum starting at 25 cm from stoma
Disclosures:
Joshua Kwon indicated no relevant financial relationships.
Anastasia Chahine indicated no relevant financial relationships.
Amelie Tiritilli indicated no relevant financial relationships.
Jason Samarasena: Applied Medical – Advisor or Review Panel Member. Boston Scientific – Consultant. Conmed – Consultant. Cook – Educational Grant. Neptune Medical – Consultant. Olympus – Consultant. Steris – Consultant.
Robert Fearn indicated no relevant financial relationships.
Valery vilchez indicated no relevant financial relationships.
Joshua Kwon, MD1, Anastasia Chahine, MD1, Amelie Tiritilli, MD2, Jason Samarasena, MD1, Robert Fearn, MD1, Valery vilchez, MD1. P3687 - Incarcerated Parastomal Hernia in the Setting of Acute Rotavirus Infection in a Patient with Crohn’s Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
