Tuesday Poster Session
Category: Interventional Endoscopy
P3700 - Safety and Efficacy of Non-Exposed Endoscopic Full-Thickness Resection Performed by Early Career Advanced Endoscopists: A Multicenter Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Natalie Wilson, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Natalie Wilson, MD1, Jenson Phung, MD1, Guarav Suryawanshi, MD1, Fouad Jaber, MD2, Danny Issa, MD3, Mohammad Bilal, MD4
1University of Minnesota, Minneapolis, MN; 2University of Missouri-Kansas City, Kansas City, MO; 3UCLA, Los Angeles, CA; 4Minneapolis VA Medical Center, Minneapolis, MN
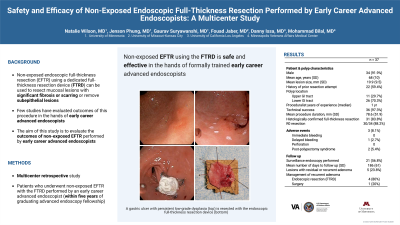
Introduction: Non-exposed endoscopic full-thickness resection (EFTR) using a dedicated full-thickness resection device (FTRD) can be used to resect mucosal lesions with significant fibrosis or scarring or remove subepithelial lesions. The FTRD is approved for use in the upper and lower gastrointestinal tract. The safety and efficacy of non-exposed EFTR has been well demonstrated in the literature; however, few studies have evaluated outcomes of this procedure in the hands of early career advanced endoscopists. The aim of this study is to evaluate the outcomes of non-exposed EFTR performed by early career advanced endoscopists.
Methods: This was a multicenter retrospective study of patients who underwent non-exposed EFTR with the FTRD performed by an early career advanced endoscopist (defined as within five years of graduating advanced endoscopy fellowship). Patient demographics, procedural data, and details pertaining to follow up endoscopy were collected. The primary outcome was technical success. This was defined as successful advancement of the FTRD to the target site followed by complete resection with the device. Secondary outcomes included R0 resection (negative deep and lateral histologic margins), rate of lesion recurrence, and adverse events.
Results: A total of 37 lesions from 34 patients were removed using the FTRD. 91.9% of patients were male with an average age of 68 years old. The most common procedure indication was residual or recurrent lesion (n = 16, 43.2%) followed by subepithelial lesion (n = 5, 13.5%), and non-lifting or scarred lesion (n = 5, 13.5%). Most lesions were located in the lower gastrointestinal (GI) tract (n = 26, 70.3%) compared to the upper GI tract (n = 11, 29.7%). The average lesion size was 19.9 mm. The median number of years of proceduralist experience was one (interquartile range: 1-2). Technical success was achieved in 97.3% of cases (n = 36). The rate of R0 resection was 88.2%. Lesion recurrence was present in five (23.8%) of 21 patients that underwent follow-up. Three adverse events occurred: two cases of post-polypectomy syndrome and one case of delayed bleeding [Table 1].
Discussion: Non-exposed endoscopic full-thickness resection using the FTRD is safe and effective in the hands of formally trained early career advanced endoscopists.
Disclosures:
Natalie Wilson, MD1, Jenson Phung, MD1, Guarav Suryawanshi, MD1, Fouad Jaber, MD2, Danny Issa, MD3, Mohammad Bilal, MD4. P3700 - Safety and Efficacy of Non-Exposed Endoscopic Full-Thickness Resection Performed by Early Career Advanced Endoscopists: A Multicenter Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Missouri-Kansas City, Kansas City, MO; 3UCLA, Los Angeles, CA; 4Minneapolis VA Medical Center, Minneapolis, MN
Introduction: Non-exposed endoscopic full-thickness resection (EFTR) using a dedicated full-thickness resection device (FTRD) can be used to resect mucosal lesions with significant fibrosis or scarring or remove subepithelial lesions. The FTRD is approved for use in the upper and lower gastrointestinal tract. The safety and efficacy of non-exposed EFTR has been well demonstrated in the literature; however, few studies have evaluated outcomes of this procedure in the hands of early career advanced endoscopists. The aim of this study is to evaluate the outcomes of non-exposed EFTR performed by early career advanced endoscopists.
Methods: This was a multicenter retrospective study of patients who underwent non-exposed EFTR with the FTRD performed by an early career advanced endoscopist (defined as within five years of graduating advanced endoscopy fellowship). Patient demographics, procedural data, and details pertaining to follow up endoscopy were collected. The primary outcome was technical success. This was defined as successful advancement of the FTRD to the target site followed by complete resection with the device. Secondary outcomes included R0 resection (negative deep and lateral histologic margins), rate of lesion recurrence, and adverse events.
Results: A total of 37 lesions from 34 patients were removed using the FTRD. 91.9% of patients were male with an average age of 68 years old. The most common procedure indication was residual or recurrent lesion (n = 16, 43.2%) followed by subepithelial lesion (n = 5, 13.5%), and non-lifting or scarred lesion (n = 5, 13.5%). Most lesions were located in the lower gastrointestinal (GI) tract (n = 26, 70.3%) compared to the upper GI tract (n = 11, 29.7%). The average lesion size was 19.9 mm. The median number of years of proceduralist experience was one (interquartile range: 1-2). Technical success was achieved in 97.3% of cases (n = 36). The rate of R0 resection was 88.2%. Lesion recurrence was present in five (23.8%) of 21 patients that underwent follow-up. Three adverse events occurred: two cases of post-polypectomy syndrome and one case of delayed bleeding [Table 1].
Discussion: Non-exposed endoscopic full-thickness resection using the FTRD is safe and effective in the hands of formally trained early career advanced endoscopists.
Disclosures:
Natalie Wilson indicated no relevant financial relationships.
Jenson Phung indicated no relevant financial relationships.
Guarav Suryawanshi indicated no relevant financial relationships.
Fouad Jaber indicated no relevant financial relationships.
Danny Issa indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant.
Natalie Wilson, MD1, Jenson Phung, MD1, Guarav Suryawanshi, MD1, Fouad Jaber, MD2, Danny Issa, MD3, Mohammad Bilal, MD4. P3700 - Safety and Efficacy of Non-Exposed Endoscopic Full-Thickness Resection Performed by Early Career Advanced Endoscopists: A Multicenter Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
