Tuesday Poster Session
Category: Interventional Endoscopy
P3729 - Pembrolizumab-Induced Cholangiopathy in the Setting of Metastatic Maxillary Sinus Squamous Cell Carcinoma
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Niloy Ghosh, MD
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Niloy Ghosh, MD1, Justin M. Joseph, MD2, Aamer Abbass, MD1, Gulshan Parasher, MD1
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM
Introduction: Cholangitis is usually caused by biliary obstruction, infection, or autoimmune processes. However, there have been several reports of rare immune checkpoint inhibitor (ICI) induced cholangitis. Here we present a case of pembrolizumab induced cholangitis in the absence of systemic symptoms.
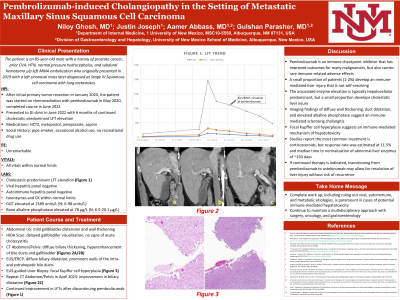
Case Description/Methods: An 85-year-old male with a history of prostate cancer and prior CVA originally presented in 2019 with a left sinonasal mass later diagnosed as Stage IV Squamous cell carcinoma with lung metastases. After resection, the patient was started on chemoradiation with pembrolizumab in May 2020. He had a severe increase in alkaline phosphatase and mild transaminitis in January 2022 in the absence of systemic symptoms. Workup included ultrasound findings of gallbladder distension and wall thickening, unremarkable HIDA scan, and CT findings of diffuse biliary thickening and hyperenhancement. Pembrolizumab was paused. Viral, autoimmune, and metabolic workup was negative. The patient underwent EUS in July 2022 after two years of pembrolizumab, with findings significant for diffuse dilation and prominent walls of the intra- and extrahepatic bile ducts thought to be due to drug induced secondary sclerosing cholangitis in the absence of endoscopic evidence of cholelithiasis or cholecystitis. An EUS guided liver biopsy showed normal liver parenchyma with focal Kupffer cell hyperplasia, suggesting drug related injury. Once one year passed after his last dose of pembrolizumab, the patient’s AST/ALT and bilirubin had normalized, and his alkaline phosphatase was significantly improved. Repeat cross-sectional imaging showed a resolution of the previously noted biliary dilatation.
Discussion: Pembrolizumab is an ICI that has improved outcomes for many malignancies, but it has rare immune-related adverse effects. While biliary complications are exceedingly rare (incidence of 1-3%), up to 7% of patients develop transaminitis. Although normally accompanied by systemic symptoms such as abdominal pain, jaundice, and fever, cholangitis may also present non-specifically with only laboratory abnormalities. Though ICI-mediated LFT elevation is typically hepatocellular, this case demonstrates cholestatic liver injury. In addition, Kupffer cell hyperplasia is atypical for sclerosing cholangitis. It is crucial in these cases to perform a complete work up, including ruling out viral, autoimmune, and metabolic etiologies, and maintain a multidisciplinary approach with surgery, oncology, and gastroenterology.
Disclosures:
Niloy Ghosh, MD1, Justin M. Joseph, MD2, Aamer Abbass, MD1, Gulshan Parasher, MD1. P3729 - Pembrolizumab-Induced Cholangiopathy in the Setting of Metastatic Maxillary Sinus Squamous Cell Carcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM
Introduction: Cholangitis is usually caused by biliary obstruction, infection, or autoimmune processes. However, there have been several reports of rare immune checkpoint inhibitor (ICI) induced cholangitis. Here we present a case of pembrolizumab induced cholangitis in the absence of systemic symptoms.
Case Description/Methods: An 85-year-old male with a history of prostate cancer and prior CVA originally presented in 2019 with a left sinonasal mass later diagnosed as Stage IV Squamous cell carcinoma with lung metastases. After resection, the patient was started on chemoradiation with pembrolizumab in May 2020. He had a severe increase in alkaline phosphatase and mild transaminitis in January 2022 in the absence of systemic symptoms. Workup included ultrasound findings of gallbladder distension and wall thickening, unremarkable HIDA scan, and CT findings of diffuse biliary thickening and hyperenhancement. Pembrolizumab was paused. Viral, autoimmune, and metabolic workup was negative. The patient underwent EUS in July 2022 after two years of pembrolizumab, with findings significant for diffuse dilation and prominent walls of the intra- and extrahepatic bile ducts thought to be due to drug induced secondary sclerosing cholangitis in the absence of endoscopic evidence of cholelithiasis or cholecystitis. An EUS guided liver biopsy showed normal liver parenchyma with focal Kupffer cell hyperplasia, suggesting drug related injury. Once one year passed after his last dose of pembrolizumab, the patient’s AST/ALT and bilirubin had normalized, and his alkaline phosphatase was significantly improved. Repeat cross-sectional imaging showed a resolution of the previously noted biliary dilatation.
Discussion: Pembrolizumab is an ICI that has improved outcomes for many malignancies, but it has rare immune-related adverse effects. While biliary complications are exceedingly rare (incidence of 1-3%), up to 7% of patients develop transaminitis. Although normally accompanied by systemic symptoms such as abdominal pain, jaundice, and fever, cholangitis may also present non-specifically with only laboratory abnormalities. Though ICI-mediated LFT elevation is typically hepatocellular, this case demonstrates cholestatic liver injury. In addition, Kupffer cell hyperplasia is atypical for sclerosing cholangitis. It is crucial in these cases to perform a complete work up, including ruling out viral, autoimmune, and metabolic etiologies, and maintain a multidisciplinary approach with surgery, oncology, and gastroenterology.
Disclosures:
Niloy Ghosh indicated no relevant financial relationships.
Justin Joseph indicated no relevant financial relationships.
Aamer Abbass indicated no relevant financial relationships.
Gulshan Parasher indicated no relevant financial relationships.
Niloy Ghosh, MD1, Justin M. Joseph, MD2, Aamer Abbass, MD1, Gulshan Parasher, MD1. P3729 - Pembrolizumab-Induced Cholangiopathy in the Setting of Metastatic Maxillary Sinus Squamous Cell Carcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
