Tuesday Poster Session
Category: Liver
P3772 - Assessing Knowledge and Management of NAFLD Amongst Residents in an Internal Medicine Practice
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Smith Agyingi, MD
University of Rochester
Rochester, NY
Presenting Author(s)
Smith Agyingi, MD1, Jonathan Huang, MD2, Alec O'Connor, MD2, Christopher Walker, MD2
1University of Rochester, Rochester, NY; 2University of Rochester Medical Center, Rochester, NY
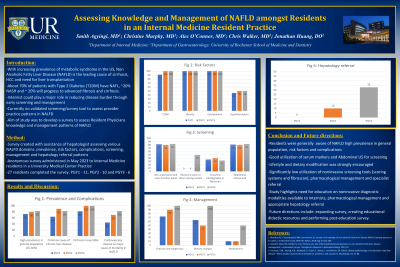
Introduction: Non-Alcoholic Fatty Liver Disease (NAFLD) is one of the leading causes of cirrhosis, hepatocellular carcinoma, and need for liver transplant in the US. Given the rising incidence and prevalence of predisposing metabolic disorders, Internists play a crucial role in reducing disease burden through screening and management. As there is currently no validated tools to assess practice patterns in NAFLD in residents, the aim of this study was to develop a survey to assess Resident Physicians’ knowledge and management trends of NALFD.
Methods: An anonymous survey was administered in May 2023 to Internal Medicine residents in a University Medical Center outpatient practice. The survey was developed with a Hepatologist and GI Fellow, and included domains assessing NAFLD prevalence, risk factors, complications, screening, management and referral patterns.
Results: For this preliminary analysis, 24/78 (31%) residents (9, 9, 6; 1st, 2nd, 3rd year) completed the survey. 18 (75%) considered NAFLD to be the major cause of chronic liver disease, and 95% recognized cirrhosis as potentially irreversible. 90% correctly identified the major risk factors T2DM, BMI >28, insulin resistance and dyslipidemia, but only 42% identified hypothyroidism. While 87% and 33% reported having used abdominal Ultrasound and fibroscan, interestingly, only 2 third year residents had screened with Fibrosis-4 or another scoring system. The majority reported having recommended lifestyle (83%) or dietary changes (58%), but only 20% had used medications. Surprisingly, only 1 third year resident had referred a patient to hepatology for overt findings of cirrhosis.
Discussion:
Our preliminary study showed that significant gaps exist in screening, management and referral patterns across IM resident training levels, including low utilization of noninvasive diagnostic tools like scoring systems and fibroscan, raising the question of awareness. Residents were generally knowledgeable about the prevalence, risk factors and complications of NAFLD. Medication use was significantly lower compared to other management strategies, however, this is unsurprising as pharmacological treatment is still in development. Finally, despite the majority identifying cirrhosis as potentially irreversible, referral trends were lower than expected. Although limited by response number, this study highlights the need for ongoing education on diagnostic modalities, medical management, and appropriate timing of hepatology referral to optimize care of NAFLD patients
Disclosures:
Smith Agyingi, MD1, Jonathan Huang, MD2, Alec O'Connor, MD2, Christopher Walker, MD2. P3772 - Assessing Knowledge and Management of NAFLD Amongst Residents in an Internal Medicine Practice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Rochester, Rochester, NY; 2University of Rochester Medical Center, Rochester, NY
Introduction: Non-Alcoholic Fatty Liver Disease (NAFLD) is one of the leading causes of cirrhosis, hepatocellular carcinoma, and need for liver transplant in the US. Given the rising incidence and prevalence of predisposing metabolic disorders, Internists play a crucial role in reducing disease burden through screening and management. As there is currently no validated tools to assess practice patterns in NAFLD in residents, the aim of this study was to develop a survey to assess Resident Physicians’ knowledge and management trends of NALFD.
Methods: An anonymous survey was administered in May 2023 to Internal Medicine residents in a University Medical Center outpatient practice. The survey was developed with a Hepatologist and GI Fellow, and included domains assessing NAFLD prevalence, risk factors, complications, screening, management and referral patterns.
Results: For this preliminary analysis, 24/78 (31%) residents (9, 9, 6; 1st, 2nd, 3rd year) completed the survey. 18 (75%) considered NAFLD to be the major cause of chronic liver disease, and 95% recognized cirrhosis as potentially irreversible. 90% correctly identified the major risk factors T2DM, BMI >28, insulin resistance and dyslipidemia, but only 42% identified hypothyroidism. While 87% and 33% reported having used abdominal Ultrasound and fibroscan, interestingly, only 2 third year residents had screened with Fibrosis-4 or another scoring system. The majority reported having recommended lifestyle (83%) or dietary changes (58%), but only 20% had used medications. Surprisingly, only 1 third year resident had referred a patient to hepatology for overt findings of cirrhosis.
Discussion:
Our preliminary study showed that significant gaps exist in screening, management and referral patterns across IM resident training levels, including low utilization of noninvasive diagnostic tools like scoring systems and fibroscan, raising the question of awareness. Residents were generally knowledgeable about the prevalence, risk factors and complications of NAFLD. Medication use was significantly lower compared to other management strategies, however, this is unsurprising as pharmacological treatment is still in development. Finally, despite the majority identifying cirrhosis as potentially irreversible, referral trends were lower than expected. Although limited by response number, this study highlights the need for ongoing education on diagnostic modalities, medical management, and appropriate timing of hepatology referral to optimize care of NAFLD patients
Disclosures:
Smith Agyingi indicated no relevant financial relationships.
Jonathan Huang indicated no relevant financial relationships.
Alec O'Connor indicated no relevant financial relationships.
Christopher Walker indicated no relevant financial relationships.
Smith Agyingi, MD1, Jonathan Huang, MD2, Alec O'Connor, MD2, Christopher Walker, MD2. P3772 - Assessing Knowledge and Management of NAFLD Amongst Residents in an Internal Medicine Practice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

