Tuesday Poster Session
Category: Liver
P3786 - Outcomes of Clostridium difficile Infection in Patients With Hepatocellular Carcinoma: A National Inpatient Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Vikash Kumar, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Vikash Kumar, MD1, Naresh kumar, MD1, Vijay Gayam, MD1, Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Raissa Nana Sede Mbakop, MD2, Dhir Gala, BS3, Fnu Vikash, MD4, Sindhu Vikash, MD5, Vinaya Gaduputi, MD6, Madhavi Reddy, MD1
1Brooklyn Hospital Center, Brooklyn, NY; 2Piedmont Athens Regional Medical Center, Athens, GA; 3American University of the Caribbean School of Medicine, Plainview, NY; 4Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY; 5Albert Einstein College of Medicine, Jacobi Medical Center, Bronx, NY; 6Blanchard Valley Health System, Findlay, OH
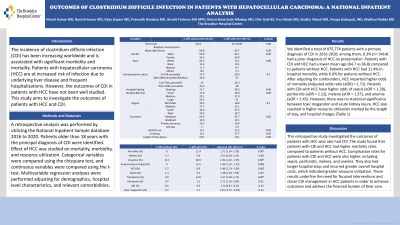
Introduction: The incidence of clostridium difficile infection (CDI) has been increasing worldwide and is associated with significant morbidity and mortality. Patients with hepatocellular carcinoma (HCC) are at increased risk of infection due to underlying liver disease and frequent hospitalizations. However, the outcomes of CDI in patients with HCC have not been well studied. This study aims to investigate the outcomes of patients with HCC and CDI.
Methods: A retrospective analysis was performed by utilizing the National Inpatient Sample database 2016 to 2020. Patients older than 18 years with the principal diagnosis of CDI were identified. Effect of HCC was studied on mortality, morbidity, and resource utilization. Categorical variables were compared using the chi-square test, and continuous variables were compared using the t- test. Multivariable regression analyses were performed adjusting for demographics, hospital-level characteristics, and relevant comorbidities.
Results: We identified a total of 875,774 patients with a primary diagnosis of CDI in 2016-2020; among them, 0.3% (n= 3414) had a prior diagnosis of HCC on presentation. Patients with CDI and HCC had a lower mean age (64.7 vs 66.8) compared to patients without HCC. Patients with HCC had 11.4% in-hospital mortality, while 6.0% for patients without HCC. After adjusting for confounders, HCC imparted higher odds of mortality (Adjusted odds ratio (aOR) = 1.71). Patients with CDI with HCC have higher odds of sepsis (aOR = 1.28), peritonitis (aOR = 2.12), melena (aOR = 1.37), and anemia (aOR = 1.45). However, there was no statistical significance between toxic megacolon and acute kidney injury. HCC also resulted in higher resource utilization marked by the length of stay, and hospital charges (Table 1).
Discussion: This retrospective study investigated the outcomes of patients with HCC who also had CDI. The study found that patients with CDI and HCC had higher mortality rates compared to patients without HCC. Complication rates for patients with CDI and HCC were also higher, including sepsis, peritonitis, melena, and anemia. They also had longer hospital stays and incurred greater overall hospital costs, which indicated greater resource utilization. These results underline the need for focused interventions and closer CDI management in HCC patients in order to enhance outcomes and address the financial burden of their care.
Disclosures:
Vikash Kumar, MD1, Naresh kumar, MD1, Vijay Gayam, MD1, Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Raissa Nana Sede Mbakop, MD2, Dhir Gala, BS3, Fnu Vikash, MD4, Sindhu Vikash, MD5, Vinaya Gaduputi, MD6, Madhavi Reddy, MD1. P3786 - Outcomes of Clostridium difficile Infection in Patients With Hepatocellular Carcinoma: A National Inpatient Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2Piedmont Athens Regional Medical Center, Athens, GA; 3American University of the Caribbean School of Medicine, Plainview, NY; 4Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY; 5Albert Einstein College of Medicine, Jacobi Medical Center, Bronx, NY; 6Blanchard Valley Health System, Findlay, OH
Introduction: The incidence of clostridium difficile infection (CDI) has been increasing worldwide and is associated with significant morbidity and mortality. Patients with hepatocellular carcinoma (HCC) are at increased risk of infection due to underlying liver disease and frequent hospitalizations. However, the outcomes of CDI in patients with HCC have not been well studied. This study aims to investigate the outcomes of patients with HCC and CDI.
Methods: A retrospective analysis was performed by utilizing the National Inpatient Sample database 2016 to 2020. Patients older than 18 years with the principal diagnosis of CDI were identified. Effect of HCC was studied on mortality, morbidity, and resource utilization. Categorical variables were compared using the chi-square test, and continuous variables were compared using the t- test. Multivariable regression analyses were performed adjusting for demographics, hospital-level characteristics, and relevant comorbidities.
Results: We identified a total of 875,774 patients with a primary diagnosis of CDI in 2016-2020; among them, 0.3% (n= 3414) had a prior diagnosis of HCC on presentation. Patients with CDI and HCC had a lower mean age (64.7 vs 66.8) compared to patients without HCC. Patients with HCC had 11.4% in-hospital mortality, while 6.0% for patients without HCC. After adjusting for confounders, HCC imparted higher odds of mortality (Adjusted odds ratio (aOR) = 1.71). Patients with CDI with HCC have higher odds of sepsis (aOR = 1.28), peritonitis (aOR = 2.12), melena (aOR = 1.37), and anemia (aOR = 1.45). However, there was no statistical significance between toxic megacolon and acute kidney injury. HCC also resulted in higher resource utilization marked by the length of stay, and hospital charges (Table 1).
Discussion: This retrospective study investigated the outcomes of patients with HCC who also had CDI. The study found that patients with CDI and HCC had higher mortality rates compared to patients without HCC. Complication rates for patients with CDI and HCC were also higher, including sepsis, peritonitis, melena, and anemia. They also had longer hospital stays and incurred greater overall hospital costs, which indicated greater resource utilization. These results underline the need for focused interventions and closer CDI management in HCC patients in order to enhance outcomes and address the financial burden of their care.
Disclosures:
Vikash Kumar indicated no relevant financial relationships.
Naresh kumar indicated no relevant financial relationships.
Vijay Gayam indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Raissa Nana Sede Mbakop indicated no relevant financial relationships.
Dhir Gala indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Sindhu Vikash indicated no relevant financial relationships.
Vinaya Gaduputi indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Vikash Kumar, MD1, Naresh kumar, MD1, Vijay Gayam, MD1, Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Raissa Nana Sede Mbakop, MD2, Dhir Gala, BS3, Fnu Vikash, MD4, Sindhu Vikash, MD5, Vinaya Gaduputi, MD6, Madhavi Reddy, MD1. P3786 - Outcomes of Clostridium difficile Infection in Patients With Hepatocellular Carcinoma: A National Inpatient Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
