Tuesday Poster Session
Category: Liver
P3793 - Socioeconomic Disparities in Alcoholic Liver Disease Outcomes
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Joanna Jiang, MD
The Ohio State Wexner Medical Center
Columbus, OH
Presenting Author(s)
Joanna Jiang, MD1, Bipul Gnyawali, BS, MD2, Elaine Shao, MD3, Mohamed I. Elsaid, PhD, MPH3, Marissa Bruce, MD4, Khalid Mumtaz, MBBS2
1The Ohio State Wexner Medical Center, Columbus, OH; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3The Ohio State University, Columbus, OH; 4Ohio State University, Columbus, OH
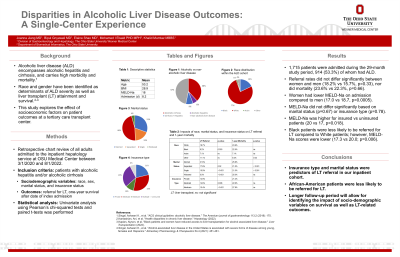
Introduction: Alcoholic liver disease (ALD) is an increasingly common cause of chronic liver disease worldwide. Previous studies on ALD have highlighted disparities in outcomes based on sex, race, and insurance status. This study sought to evaluate socioeconomic factors as predictors of outcomes at a tertiary care transplant center.
Methods: A retrospective chart review was conducted for all adults who were admitted to the inpatient hepatology service at our hospital between 3/1/2020 and 8/1/2022. Sociodemographic variables including race, sex, marital status, employment, and insurance status were collected. Outcomes included referral for liver transplantation (LT) and one-year mortality after index admission. Univariate analyses were conducted with Pearson’s chi-squared test.
Results: Of 1,715 individuals admitted during the study period, 813 (47.4%) had alcoholic cirrhosis, 258 (15%) had alcoholic hepatitis, and 801 had non-alcoholic liver disease. The mean age was 53.2 years. Patients were predominantly male (67.6%) and Caucasian (76.6%).
There was no significant difference in LT referral rate between females and males (18.2% and 15.7%, p=0.33), and one-year mortality was comparable (23.6% and 22.3%, p=0.66). White patients were significantly more likely to be referred for LT than Black patients (18.7% vs 9.15%, p=0.003). However, one-year mortality did not differ significantly by race (p=0.08). Married patients were also significantly more likely to be referred for LT than those who were single (31.6% vs 15.9%, p< 0.001), divorced (17.9%, p=0.02), or widowed (0%, p< 0.001). This corresponded to similarly significant differences in mortality (Table). Rates of LT referral were significantly higher in patients with private insurance than Medicare or Medicaid (21.7% vs 10.4% vs 14.6%, p < 0.001). However, mortality did not differ significantly by insurance status (Medicaid, Medicare, or private), which diverges from previous literature.
Discussion: Race and insurance status remain significant predictors of LT referral in our inpatient ALD population. Social support predicts higher referral rates and improved survival. Multivariate analysis is needed to control for other determinants, particularly MELD-Na score, and to quantify effect sizes of socioeconomic variables in impacting ALD outcomes.
Disclosures:
Joanna Jiang, MD1, Bipul Gnyawali, BS, MD2, Elaine Shao, MD3, Mohamed I. Elsaid, PhD, MPH3, Marissa Bruce, MD4, Khalid Mumtaz, MBBS2. P3793 - Socioeconomic Disparities in Alcoholic Liver Disease Outcomes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1The Ohio State Wexner Medical Center, Columbus, OH; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3The Ohio State University, Columbus, OH; 4Ohio State University, Columbus, OH
Introduction: Alcoholic liver disease (ALD) is an increasingly common cause of chronic liver disease worldwide. Previous studies on ALD have highlighted disparities in outcomes based on sex, race, and insurance status. This study sought to evaluate socioeconomic factors as predictors of outcomes at a tertiary care transplant center.
Methods: A retrospective chart review was conducted for all adults who were admitted to the inpatient hepatology service at our hospital between 3/1/2020 and 8/1/2022. Sociodemographic variables including race, sex, marital status, employment, and insurance status were collected. Outcomes included referral for liver transplantation (LT) and one-year mortality after index admission. Univariate analyses were conducted with Pearson’s chi-squared test.
Results: Of 1,715 individuals admitted during the study period, 813 (47.4%) had alcoholic cirrhosis, 258 (15%) had alcoholic hepatitis, and 801 had non-alcoholic liver disease. The mean age was 53.2 years. Patients were predominantly male (67.6%) and Caucasian (76.6%).
There was no significant difference in LT referral rate between females and males (18.2% and 15.7%, p=0.33), and one-year mortality was comparable (23.6% and 22.3%, p=0.66). White patients were significantly more likely to be referred for LT than Black patients (18.7% vs 9.15%, p=0.003). However, one-year mortality did not differ significantly by race (p=0.08). Married patients were also significantly more likely to be referred for LT than those who were single (31.6% vs 15.9%, p< 0.001), divorced (17.9%, p=0.02), or widowed (0%, p< 0.001). This corresponded to similarly significant differences in mortality (Table). Rates of LT referral were significantly higher in patients with private insurance than Medicare or Medicaid (21.7% vs 10.4% vs 14.6%, p < 0.001). However, mortality did not differ significantly by insurance status (Medicaid, Medicare, or private), which diverges from previous literature.
Discussion: Race and insurance status remain significant predictors of LT referral in our inpatient ALD population. Social support predicts higher referral rates and improved survival. Multivariate analysis is needed to control for other determinants, particularly MELD-Na score, and to quantify effect sizes of socioeconomic variables in impacting ALD outcomes.
Disclosures:
Joanna Jiang indicated no relevant financial relationships.
Bipul Gnyawali indicated no relevant financial relationships.
Elaine Shao indicated no relevant financial relationships.
Mohamed Elsaid indicated no relevant financial relationships.
Marissa Bruce indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Joanna Jiang, MD1, Bipul Gnyawali, BS, MD2, Elaine Shao, MD3, Mohamed I. Elsaid, PhD, MPH3, Marissa Bruce, MD4, Khalid Mumtaz, MBBS2. P3793 - Socioeconomic Disparities in Alcoholic Liver Disease Outcomes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
